Monday Poster Session
Category: IBD
P2555 - Impact of the COVID-19 Pandemic on Inflammatory Bowel Disease-Related Mortality: An Analysis of Disparities 2020-2022
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Aarzoo Kumar, BS
Banner - University of Arizona
Tucson, AZ
Presenting Author(s)
Aarzoo Kumar, BS1, Rama Mouhaffel, MD1, Nazli Begum Ozturk, MD2, Ramzi Ibrahim, MD1, Hoang Nhat Pham, MD1
1Banner - University of Arizona, Tucson, AZ; 2Corewell Health William Beaumont University Hospital, Royal Oak, MI
Introduction: Inflammatory bowel disease (IBD) affects approximately 1.4 million Americans and carries a significant healthcare burden in the US. Little is known regarding the COVID-19 pandemic's impact on IBD-related mortality and disparities.
Methods: We analyzed IBD mortality data using ICD-10 codes K50-K51 from the CDC database spanning from 1999 to 2022. Average annual percentage change (AAPC) from 1999-2019 was used to calculate the projected age-adjusted mortality rate (AAMR) in 2020-2022, compared to the actual death rates to estimate pandemic-attributed excess deaths and percent of excess AAMR.
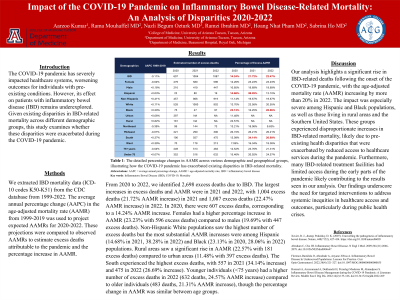
Results: During the COVID-19 pandemic, a total of 2,698 excess IBD-related deaths was recorded, with the most significant increases occurring in 2021 (1,004 excess deaths, 21.72% AAMR rise) and 2022 (1,087 excess deaths, 22.47% AAMR rise). From 2020 to 2022, females contributed higher number excess deaths and experienced higher AAMR increases (12.26%, 23.23%, and 23.23%, respectively). Race and ethnicity stratification revealed the largest AAMR increases were among Hispanic (14.68% in 2021, 38.28% in 2022) and Black (23.13% in 2020, 28.06% in 2022) populations. Rural areas saw a significant rise in AAMR (22.57% with 181 excess deaths) compared to urban areas (11.48% with 397 excess deaths) in 2020. Southern US region had the highest excess deaths, with 557 in 2021 (34.14% increase) and 475 in 2022 (26.69% increase). Individuals under 75 years had higher excess deaths and increase in AAMR were observed in in 2020 (352 excess deaths, 15.46% rise) and 2022 (632 excess deaths, 24.57% rise) compared to those >75 years.
Discussion: Our analysis highlights a significant rise in IBD-related deaths following the onset of the COVID-19 pandemic, notable in 2021 and 2022. The impact was most pronounced among Hispanic and Black populations, as well as residents of rural areas and Southern US regions. These groups experienced disproportionate increases in IBD-related mortality, likely due to pre-existing health disparities that were exacerbated by reduced access to healthcare services during the pandemic. Furthermore, many IBD-related treatment facilities had limited access during the early parts of the pandemic likely contributing to the results seen in our analysis. Our findings underscore the need for targeted interventions to address systemic inequities in healthcare access and outcomes, particularly during public health crises.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Aarzoo Kumar, BS1, Rama Mouhaffel, MD1, Nazli Begum Ozturk, MD2, Ramzi Ibrahim, MD1, Hoang Nhat Pham, MD1. P2555 - Impact of the COVID-19 Pandemic on Inflammatory Bowel Disease-Related Mortality: An Analysis of Disparities 2020-2022, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Banner - University of Arizona, Tucson, AZ; 2Corewell Health William Beaumont University Hospital, Royal Oak, MI
Introduction: Inflammatory bowel disease (IBD) affects approximately 1.4 million Americans and carries a significant healthcare burden in the US. Little is known regarding the COVID-19 pandemic's impact on IBD-related mortality and disparities.
Methods: We analyzed IBD mortality data using ICD-10 codes K50-K51 from the CDC database spanning from 1999 to 2022. Average annual percentage change (AAPC) from 1999-2019 was used to calculate the projected age-adjusted mortality rate (AAMR) in 2020-2022, compared to the actual death rates to estimate pandemic-attributed excess deaths and percent of excess AAMR.
Results: During the COVID-19 pandemic, a total of 2,698 excess IBD-related deaths was recorded, with the most significant increases occurring in 2021 (1,004 excess deaths, 21.72% AAMR rise) and 2022 (1,087 excess deaths, 22.47% AAMR rise). From 2020 to 2022, females contributed higher number excess deaths and experienced higher AAMR increases (12.26%, 23.23%, and 23.23%, respectively). Race and ethnicity stratification revealed the largest AAMR increases were among Hispanic (14.68% in 2021, 38.28% in 2022) and Black (23.13% in 2020, 28.06% in 2022) populations. Rural areas saw a significant rise in AAMR (22.57% with 181 excess deaths) compared to urban areas (11.48% with 397 excess deaths) in 2020. Southern US region had the highest excess deaths, with 557 in 2021 (34.14% increase) and 475 in 2022 (26.69% increase). Individuals under 75 years had higher excess deaths and increase in AAMR were observed in in 2020 (352 excess deaths, 15.46% rise) and 2022 (632 excess deaths, 24.57% rise) compared to those >75 years.
Discussion: Our analysis highlights a significant rise in IBD-related deaths following the onset of the COVID-19 pandemic, notable in 2021 and 2022. The impact was most pronounced among Hispanic and Black populations, as well as residents of rural areas and Southern US regions. These groups experienced disproportionate increases in IBD-related mortality, likely due to pre-existing health disparities that were exacerbated by reduced access to healthcare services during the pandemic. Furthermore, many IBD-related treatment facilities had limited access during the early parts of the pandemic likely contributing to the results seen in our analysis. Our findings underscore the need for targeted interventions to address systemic inequities in healthcare access and outcomes, particularly during public health crises.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Aarzoo Kumar indicated no relevant financial relationships.
Rama Mouhaffel indicated no relevant financial relationships.
Nazli Begum Ozturk indicated no relevant financial relationships.
Ramzi Ibrahim indicated no relevant financial relationships.
Hoang Nhat Pham indicated no relevant financial relationships.
Aarzoo Kumar, BS1, Rama Mouhaffel, MD1, Nazli Begum Ozturk, MD2, Ramzi Ibrahim, MD1, Hoang Nhat Pham, MD1. P2555 - Impact of the COVID-19 Pandemic on Inflammatory Bowel Disease-Related Mortality: An Analysis of Disparities 2020-2022, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
