Monday Poster Session
Category: IBD
P2556 - Contemporary Trends and Outcomes of Recurrent VTE in Elderly IBD Patients With Prior MACCE: Insights From Nationwide Analysis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SK
Sai Gautham Kanagala, MD
NYC Health + Hospitals/Metropolitan
New York, NY
Presenting Author(s)
Sai Gautham Kanagala, MD1, Nikitha Chellapuram, MD2, Ahmad Al Homaid, MD3, Supti Dev Nath, MBBS4, Srikara Gondhi, MBBS5, Rewanth Katamreddy, MD6, Rupak Desai, MBBS7
1NYC Health + Hospitals/Metropolitan, New York, NY; 2Centinela Hospital Medical Center, Los Angeles, CA; 3Nazareth Hospital, Philadelphia, PA; 4Johns Hopkins University, Baltimore, MD; 5Advocate Illinois Masonic Medical Center, Chicago, IL; 6NYMC - Saint Michael's Medical Center, New Jersey, NJ; 7Outcomes Research, Atlanta, GA
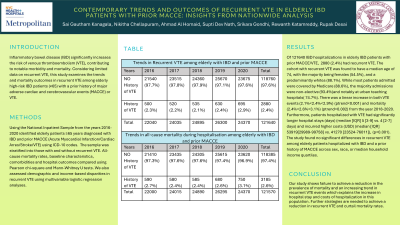
Introduction: Inflammatory bowel disease (IBD) significantly increases the risk of venous thromboembolism (VTE), contributing to notable morbidity and mortality. Considering limited data on recurrent VTE, this study examines the trends and mortality outcomes in recurrent VTE among elderly high-risk IBD patients (≥65) with a prior history of major adverse cardiac and cerebrovascular events (MACCE) or VTE.
Methods: Using the National Inpatient Sample from the years 2016-2020 identified elderly patients ≥65 years diagnosed with IBD and prior MACCE (Acute Myocardial Infarction/Cardiac Arres/Stroke/VTE) using ICD-10 codes. The sample was stratified into those with and without recurrent VTE. All-cause mortality rates, baseline characteristics, comorbidities and hospital outcomes compared using Pearson chi-square and Mann-Whitney U tests. We also assessed demographic and income-based disparities in recurrent VTE using multivariable logistic regression analyses.
Results: Of 121640 IBD hospitalizations in elderly IBD patients with prior MACCE/VTE, 2880 (2.4%) had recurrent VTE. The cohort with recurrent VTE was found to have a median age of 74, with the majority being females (54.5%), and predominantly whites (88.1%). While most patients admitted were covered by Medicare (88.6%), the majority admissions were non-elective (93.4%)and notably at urban teaching hospitals( 74.7%). There was a linear increase in both VTE events (2.1%< 2.4%< 2.9%) (ptrend< 0.001) and mortality (2.4%< 2.6%< 3.1%) (ptrend=0.002) from the year 2018-2020. Furthermore, patients hospitalized with VTE had significantly longer hospital stays (median [IQR] 5 [3-9] vs. 4 [2-7] days) and incurred higher costs (USD) (median [IQR] 53919[29989-99758] vs. 41270 [23524-76011]), (p< 0.001). The study found no significant differences in recurrent VTE among elderly patients hospitalized with IBD and a prior history of MACCE across sex, race, or median household income quartiles.
Discussion: Our study shows failure to achieve a reduction in the prevalence of mortality and an increasing trend in recurrent VTE events which explains the increase in hospital stay and costs of hospitalization in this population. Further strategies are needed to achieve a reduction in recurrent VTE and curtail mortality rates.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sai Gautham Kanagala, MD1, Nikitha Chellapuram, MD2, Ahmad Al Homaid, MD3, Supti Dev Nath, MBBS4, Srikara Gondhi, MBBS5, Rewanth Katamreddy, MD6, Rupak Desai, MBBS7. P2556 - Contemporary Trends and Outcomes of Recurrent VTE in Elderly IBD Patients With Prior MACCE: Insights From Nationwide Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1NYC Health + Hospitals/Metropolitan, New York, NY; 2Centinela Hospital Medical Center, Los Angeles, CA; 3Nazareth Hospital, Philadelphia, PA; 4Johns Hopkins University, Baltimore, MD; 5Advocate Illinois Masonic Medical Center, Chicago, IL; 6NYMC - Saint Michael's Medical Center, New Jersey, NJ; 7Outcomes Research, Atlanta, GA
Introduction: Inflammatory bowel disease (IBD) significantly increases the risk of venous thromboembolism (VTE), contributing to notable morbidity and mortality. Considering limited data on recurrent VTE, this study examines the trends and mortality outcomes in recurrent VTE among elderly high-risk IBD patients (≥65) with a prior history of major adverse cardiac and cerebrovascular events (MACCE) or VTE.
Methods: Using the National Inpatient Sample from the years 2016-2020 identified elderly patients ≥65 years diagnosed with IBD and prior MACCE (Acute Myocardial Infarction/Cardiac Arres/Stroke/VTE) using ICD-10 codes. The sample was stratified into those with and without recurrent VTE. All-cause mortality rates, baseline characteristics, comorbidities and hospital outcomes compared using Pearson chi-square and Mann-Whitney U tests. We also assessed demographic and income-based disparities in recurrent VTE using multivariable logistic regression analyses.
Results: Of 121640 IBD hospitalizations in elderly IBD patients with prior MACCE/VTE, 2880 (2.4%) had recurrent VTE. The cohort with recurrent VTE was found to have a median age of 74, with the majority being females (54.5%), and predominantly whites (88.1%). While most patients admitted were covered by Medicare (88.6%), the majority admissions were non-elective (93.4%)and notably at urban teaching hospitals( 74.7%). There was a linear increase in both VTE events (2.1%< 2.4%< 2.9%) (ptrend< 0.001) and mortality (2.4%< 2.6%< 3.1%) (ptrend=0.002) from the year 2018-2020. Furthermore, patients hospitalized with VTE had significantly longer hospital stays (median [IQR] 5 [3-9] vs. 4 [2-7] days) and incurred higher costs (USD) (median [IQR] 53919[29989-99758] vs. 41270 [23524-76011]), (p< 0.001). The study found no significant differences in recurrent VTE among elderly patients hospitalized with IBD and a prior history of MACCE across sex, race, or median household income quartiles.
Discussion: Our study shows failure to achieve a reduction in the prevalence of mortality and an increasing trend in recurrent VTE events which explains the increase in hospital stay and costs of hospitalization in this population. Further strategies are needed to achieve a reduction in recurrent VTE and curtail mortality rates.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sai Gautham Kanagala indicated no relevant financial relationships.
Nikitha Chellapuram indicated no relevant financial relationships.
Ahmad Al Homaid indicated no relevant financial relationships.
Supti Dev Nath indicated no relevant financial relationships.
Srikara Gondhi indicated no relevant financial relationships.
Rewanth Katamreddy indicated no relevant financial relationships.
Rupak Desai indicated no relevant financial relationships.
Sai Gautham Kanagala, MD1, Nikitha Chellapuram, MD2, Ahmad Al Homaid, MD3, Supti Dev Nath, MBBS4, Srikara Gondhi, MBBS5, Rewanth Katamreddy, MD6, Rupak Desai, MBBS7. P2556 - Contemporary Trends and Outcomes of Recurrent VTE in Elderly IBD Patients With Prior MACCE: Insights From Nationwide Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
