Monday Poster Session
Category: GI Bleeding
P2463 - An Analysis of the Compliance of 2 Large-Bore Intravenous Lines in Gastrointestinal Bleeding
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
William KB Boateng, MD
Jersey City Medical Center
Bayonne, NJ
Presenting Author(s)
William KB. Boateng, MD1, Fomengia Joseph. Nkeangu, MD2, Sarpong Boateng, MD, MPH3, Mannat Kaur. Bhatia, MD4, Kosisochukwu Ezeh, MD5
1Jersey City Medical Center, Bayonne, NJ; 2Jersey City Medical Center, Jersey City, NJ; 3Yale New Haven Health, Bridgeport Hospital, Bridgeport, CT; 4Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 5Marshall University, Charleston, WV
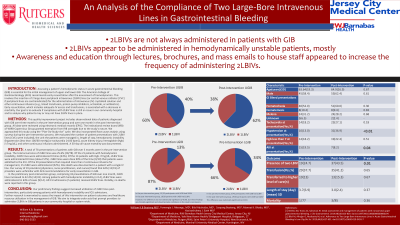
Introduction: Early hemodynamic assessment and resuscitation are critical in the management of acute gastrointestinal bleeding (GIB). The American College of Gastroenterology (ACG) recommends the insertion of two large-bore intravenous (2LBIV) lines for effective administration of fluids and medications. Despite these guidelines, compliance with 2LBIV line placement remains suboptimal. This quality improvement project aimed to evaluate adherence to the ACG recommendations for 2LBIV line placement in a community hospital and to identify factors influencing compliance.
Methods: We conducted a pre- and post-intervention study over four months, using data from electronic medical records for patients with GIB. The pre-intervention phase included 78 patient presentations over three months, while the post-intervention phase encompassed 33 presentations over one month. Data collected included the presence of 2LBIV lines, patient unit (e.g., ICU), hemodynamic stability, hemoglobin levels, need for continuous infusions, and 30-day all-cause mortality. Root cause analysis and provider surveys assessed awareness of ACG guidelines.
Results: In the pre-intervention group, only 25.6% (20/78) of patients had 2LBIV lines inserted. For patients with hemodynamic instability, 2LBIV lines were placed in 43% (9/21) of cases, and in 57% (8/14) of those with hemoglobin levels below 7 mg/dL. ICU patients received 2LBIV lines 90% (9/10) of the time. The post-intervention group showed an increase in compliance, with 42.4% (14/33) of patients receiving 2LBIV lines, and 64% (9/14) of those with hemodynamic instability being properly managed. All ICU admissions (5 patients) received 2LBIV lines. Provider surveys revealed that 63% (12/19) were unaware of ACG's resuscitation guidelines.
Discussion: Our findings suggest an increase in the utilization of 2LBIV lines post-intervention, particularly among patients with hemodynamic instability and ICU admissions. Further research is warranted to assess the impact of this intervention on patient outcomes and healthcare resource utilization in the management of GIB. Our aim is to integrate order sets that prompt providers to administer 2LBIVs in GIB patients in our community hospital or system-wide.
Disclosures:
William KB. Boateng, MD1, Fomengia Joseph. Nkeangu, MD2, Sarpong Boateng, MD, MPH3, Mannat Kaur. Bhatia, MD4, Kosisochukwu Ezeh, MD5. P2463 - An Analysis of the Compliance of 2 Large-Bore Intravenous Lines in Gastrointestinal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Jersey City Medical Center, Bayonne, NJ; 2Jersey City Medical Center, Jersey City, NJ; 3Yale New Haven Health, Bridgeport Hospital, Bridgeport, CT; 4Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 5Marshall University, Charleston, WV
Introduction: Early hemodynamic assessment and resuscitation are critical in the management of acute gastrointestinal bleeding (GIB). The American College of Gastroenterology (ACG) recommends the insertion of two large-bore intravenous (2LBIV) lines for effective administration of fluids and medications. Despite these guidelines, compliance with 2LBIV line placement remains suboptimal. This quality improvement project aimed to evaluate adherence to the ACG recommendations for 2LBIV line placement in a community hospital and to identify factors influencing compliance.
Methods: We conducted a pre- and post-intervention study over four months, using data from electronic medical records for patients with GIB. The pre-intervention phase included 78 patient presentations over three months, while the post-intervention phase encompassed 33 presentations over one month. Data collected included the presence of 2LBIV lines, patient unit (e.g., ICU), hemodynamic stability, hemoglobin levels, need for continuous infusions, and 30-day all-cause mortality. Root cause analysis and provider surveys assessed awareness of ACG guidelines.
Results: In the pre-intervention group, only 25.6% (20/78) of patients had 2LBIV lines inserted. For patients with hemodynamic instability, 2LBIV lines were placed in 43% (9/21) of cases, and in 57% (8/14) of those with hemoglobin levels below 7 mg/dL. ICU patients received 2LBIV lines 90% (9/10) of the time. The post-intervention group showed an increase in compliance, with 42.4% (14/33) of patients receiving 2LBIV lines, and 64% (9/14) of those with hemodynamic instability being properly managed. All ICU admissions (5 patients) received 2LBIV lines. Provider surveys revealed that 63% (12/19) were unaware of ACG's resuscitation guidelines.
Discussion: Our findings suggest an increase in the utilization of 2LBIV lines post-intervention, particularly among patients with hemodynamic instability and ICU admissions. Further research is warranted to assess the impact of this intervention on patient outcomes and healthcare resource utilization in the management of GIB. Our aim is to integrate order sets that prompt providers to administer 2LBIVs in GIB patients in our community hospital or system-wide.
Disclosures:
William Boateng indicated no relevant financial relationships.
Fomengia Nkeangu indicated no relevant financial relationships.
Sarpong Boateng indicated no relevant financial relationships.
Mannat Bhatia indicated no relevant financial relationships.
Kosisochukwu Ezeh indicated no relevant financial relationships.
William KB. Boateng, MD1, Fomengia Joseph. Nkeangu, MD2, Sarpong Boateng, MD, MPH3, Mannat Kaur. Bhatia, MD4, Kosisochukwu Ezeh, MD5. P2463 - An Analysis of the Compliance of 2 Large-Bore Intravenous Lines in Gastrointestinal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

