Monday Poster Session
Category: GI Bleeding
P2467 - Percutaneous Coronary Intervention in Cancer Patients: Assessing 30-Day Bleeding Readmissions
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Silpa Choday, MD
Creighton University School of Medicine
Phoenix, AZ
Presenting Author(s)
Silpa Choday, MD1, Gautam Maddineni, MD2, Tamer Zahdeh, MD3, Diana Zamora, MD1, Miguel Gonzalez, MD1
1Creighton University School of Medicine, Phoenix, AZ; 2Florida State University, Cape Coral, FL; 3Montefiore St. Luke's Cornwall, New York, NY
Introduction: Percutaneous coronary intervention (PCI) is a procedure used to treat coronary artery disease. Cancer patients frequently present with comorbidities, including cardiovascular disease, which may necessitate PCI. However, oncologic treatments can increase the risk of complications during and after PCI. One such complication is upper gastrointestinal (GI) bleeding, which can occur due to concomitant use of anticoagulant and antiplatelet medications during PCI, as well as underlying cancer-related factors such as tumor invasion, mucosal damage or coagulopathy. This study examined the readmission rates for non-variceal UGI bleeding post PCI.
Methods: This retrospective cohort study analyzed cancer patients who underwent PCI and were readmitted within 30 days for GI bleed. Data was acquired from the Nationwide Readmission Database (NRD) from 2016 to 2020 and analyzed using multivariable logistic regression.
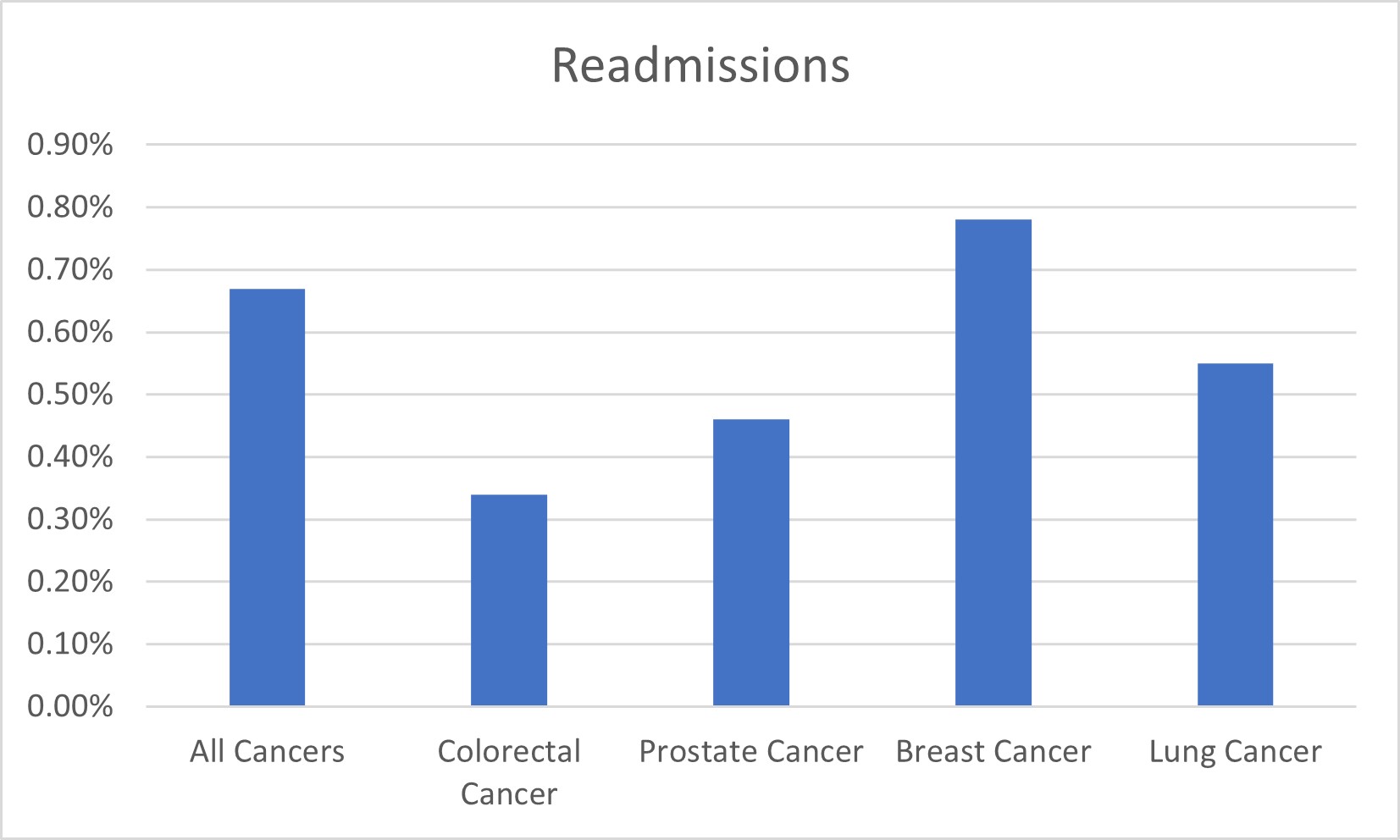
Results: A total of 2,705,049 patients were included in the analysis.8,890 (0.3%) patients were readmitted for GI bleeding within 30 days post PCI (P< 0.001). Over the study period, there was a slight uptick in the trend of readmissions for bleeding, rising from 0.3% to 0.4%. Those readmitted were more likely to be male (P< 0.001), aged >61 years (P< 0.001), and covered by Medicare insurance (P< 0.001). Notably, patients readmitted for GI bleeding within 30 days post-PCI had a significantly higher incidence of cancer diagnosis (58% with cancer vs 29% without, P< 0.001). Furthermore, the likelihood of 30-day readmission for bleeding after PCI was notably elevated in patients with active cancer compared to those without (0.66% vs 0.19%) (P< 0.001). Among cancer types, breast cancer exhibited the highest readmission rates (0.78% vs 0.33%), followed by lung cancer (0.55% vs 0.33%), prostate cancer (0.46% vs 0.33%), and colorectal cancer (0.34% vs 0.33%) (P< 0.001). The average time to GI bleeding readmission ranged from 9.4 days for colorectal cancer to 13.3 days for breast cancer, with an overall average of 12.7 days across all cancer types.
Discussion: PCI in cancer patients presents a complex clinical scenario with multidisciplinary approach, integrating cardiology, oncology, and gastroenterology expertise. Post-PCI, individuals with cancer face heightened susceptibility to readmissions due to bleeding events, with the degree of risk influenced by cancer type, sex, age and active cancer.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Silpa Choday, MD1, Gautam Maddineni, MD2, Tamer Zahdeh, MD3, Diana Zamora, MD1, Miguel Gonzalez, MD1. P2467 - Percutaneous Coronary Intervention in Cancer Patients: Assessing 30-Day Bleeding Readmissions, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Creighton University School of Medicine, Phoenix, AZ; 2Florida State University, Cape Coral, FL; 3Montefiore St. Luke's Cornwall, New York, NY
Introduction: Percutaneous coronary intervention (PCI) is a procedure used to treat coronary artery disease. Cancer patients frequently present with comorbidities, including cardiovascular disease, which may necessitate PCI. However, oncologic treatments can increase the risk of complications during and after PCI. One such complication is upper gastrointestinal (GI) bleeding, which can occur due to concomitant use of anticoagulant and antiplatelet medications during PCI, as well as underlying cancer-related factors such as tumor invasion, mucosal damage or coagulopathy. This study examined the readmission rates for non-variceal UGI bleeding post PCI.
Methods: This retrospective cohort study analyzed cancer patients who underwent PCI and were readmitted within 30 days for GI bleed. Data was acquired from the Nationwide Readmission Database (NRD) from 2016 to 2020 and analyzed using multivariable logistic regression.
Results: A total of 2,705,049 patients were included in the analysis.8,890 (0.3%) patients were readmitted for GI bleeding within 30 days post PCI (P< 0.001). Over the study period, there was a slight uptick in the trend of readmissions for bleeding, rising from 0.3% to 0.4%. Those readmitted were more likely to be male (P< 0.001), aged >61 years (P< 0.001), and covered by Medicare insurance (P< 0.001). Notably, patients readmitted for GI bleeding within 30 days post-PCI had a significantly higher incidence of cancer diagnosis (58% with cancer vs 29% without, P< 0.001). Furthermore, the likelihood of 30-day readmission for bleeding after PCI was notably elevated in patients with active cancer compared to those without (0.66% vs 0.19%) (P< 0.001). Among cancer types, breast cancer exhibited the highest readmission rates (0.78% vs 0.33%), followed by lung cancer (0.55% vs 0.33%), prostate cancer (0.46% vs 0.33%), and colorectal cancer (0.34% vs 0.33%) (P< 0.001). The average time to GI bleeding readmission ranged from 9.4 days for colorectal cancer to 13.3 days for breast cancer, with an overall average of 12.7 days across all cancer types.
Discussion: PCI in cancer patients presents a complex clinical scenario with multidisciplinary approach, integrating cardiology, oncology, and gastroenterology expertise. Post-PCI, individuals with cancer face heightened susceptibility to readmissions due to bleeding events, with the degree of risk influenced by cancer type, sex, age and active cancer.
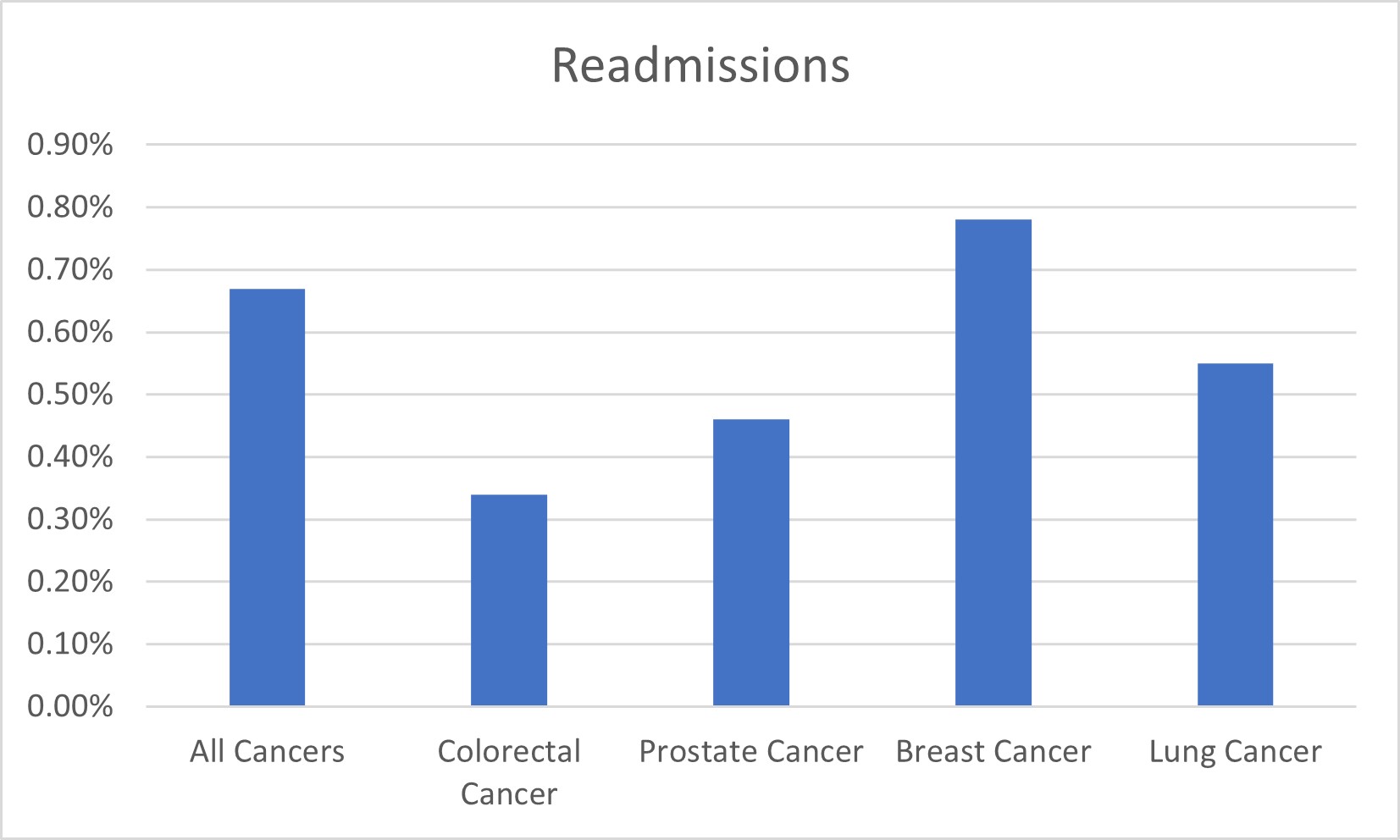
Figure: Readmissions by cancer type
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Silpa Choday indicated no relevant financial relationships.
Gautam Maddineni indicated no relevant financial relationships.
Tamer Zahdeh indicated no relevant financial relationships.
Diana Zamora indicated no relevant financial relationships.
Miguel Gonzalez indicated no relevant financial relationships.
Silpa Choday, MD1, Gautam Maddineni, MD2, Tamer Zahdeh, MD3, Diana Zamora, MD1, Miguel Gonzalez, MD1. P2467 - Percutaneous Coronary Intervention in Cancer Patients: Assessing 30-Day Bleeding Readmissions, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
