Monday Poster Session
Category: GI Bleeding
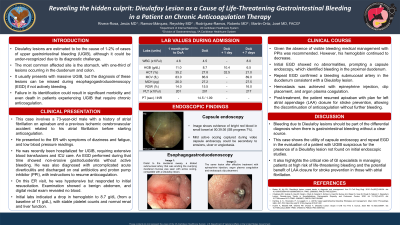
P2473 - Revealing the Hidden Culprit: Dieulafoy Lesion as a Cause of Life-Threatening Gastrointestinal Bleeding in a Patient on Chronic Anticoagulation Therapy
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Jesus Rivera-Rosa, MD
VA Caribbean Healthcare System
Bayamon, PR
Presenting Author(s)
Jesus Rivera-Rosa, MD1, Reyshley Ramos-Márquez, MD2, Roberto Rodriguez-Ramos, MD2, Jose Martin-Ortiz, MD, FACG2
1VA Caribbean Healthcare System, Bayamon, Puerto Rico; 2VA Caribbean Healthcare System, San Juan, Puerto Rico
Introduction: Dieulafoy lesions are a known cause of upper gastrointestinal bleeding (UGIB), however their diagnosis can be challenging as these lesions can be missed during esophagogastroduodenoscopy (EGD) if not actively bleeding. Failure in its identification could result in significant morbidity and even death in patients experiencing UGIB that require chronic anticoagulation.
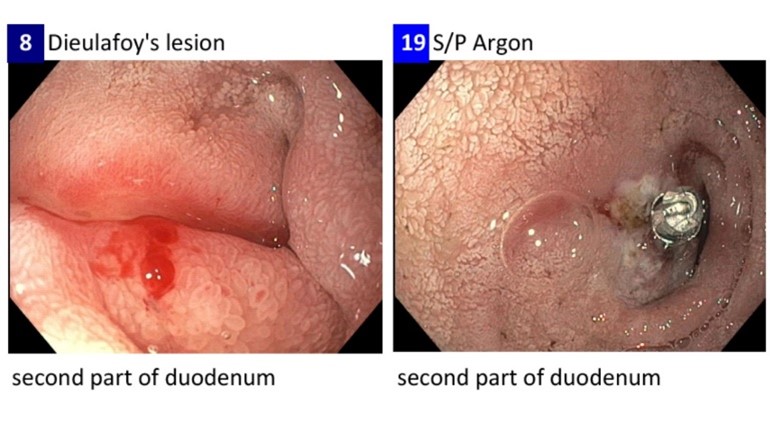
Case Description/Methods: This case involves a 73-year-old male with a history of atrial fibrillation on apixaban and a previous ischemic cerebrovascular accident related to his atrial fibrillation before starting anticoagulation. He presented to the ER with symptoms of dizziness and fatigue, and low blood pressure readings. He had recently been hospitalized for UGIB, requiring extensive blood transfusions and ICU care. An EGD performed during that admission showed non-erosive gastroduodenitis without active bleeding. He was also diagnosed with uncomplicated acute diverticulitis and discharged on oral antibiotics and proton pump inhibitor (PPI), with instructions to resume anticoagulation. After discharge patient denied further bleeding episodes, abdominal pain, nausea/vomiting. Evaluation at ER revealed a hypotensive patient that responded to initial resuscitation interventions. Examination showed a benign abdomen and digital rectal exam revealed no blood. Initial labs indicated a drop in hemoglobin to 8.7 g/dL (from a baseline of 11 g/dL), with stable platelet counts and normal renal and liver function. Patient was admitted and GI service consulted. EGD performed failed to identify a source of bleeding. Subsequently, capsule endoscopy was performed and showed a focus of active bleeding in the proximal duodenum. EGD was repeated confirming the presence of a dilated submucosal artery with active oozing in the second portion of the duodenum compatible with a Dieulafoy lesion. Hemostasis was achieved after injection of epinephrine, clip placement, and argon plasma coagulation. Post-treatment, the patient resumed apixaban with plan for left atrial appendage (LAA) closure for stroke prevention, allowing the discontinuation of anticoagulation without further bleeding.
Discussion: This case demonstrates the value of capsule endoscopy for detecting Dieulafoy lesions not identified on EGD. It also highlights the critical role of GI specialists in managing patients at high risk of life-threatening bleeding and the potential benefit of LAA closure for stroke prevention in those with atrial fibrillation.
Disclosures:
Jesus Rivera-Rosa, MD1, Reyshley Ramos-Márquez, MD2, Roberto Rodriguez-Ramos, MD2, Jose Martin-Ortiz, MD, FACG2. P2473 - Revealing the Hidden Culprit: Dieulafoy Lesion as a Cause of Life-Threatening Gastrointestinal Bleeding in a Patient on Chronic Anticoagulation Therapy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1VA Caribbean Healthcare System, Bayamon, Puerto Rico; 2VA Caribbean Healthcare System, San Juan, Puerto Rico
Introduction: Dieulafoy lesions are a known cause of upper gastrointestinal bleeding (UGIB), however their diagnosis can be challenging as these lesions can be missed during esophagogastroduodenoscopy (EGD) if not actively bleeding. Failure in its identification could result in significant morbidity and even death in patients experiencing UGIB that require chronic anticoagulation.
Case Description/Methods: This case involves a 73-year-old male with a history of atrial fibrillation on apixaban and a previous ischemic cerebrovascular accident related to his atrial fibrillation before starting anticoagulation. He presented to the ER with symptoms of dizziness and fatigue, and low blood pressure readings. He had recently been hospitalized for UGIB, requiring extensive blood transfusions and ICU care. An EGD performed during that admission showed non-erosive gastroduodenitis without active bleeding. He was also diagnosed with uncomplicated acute diverticulitis and discharged on oral antibiotics and proton pump inhibitor (PPI), with instructions to resume anticoagulation. After discharge patient denied further bleeding episodes, abdominal pain, nausea/vomiting. Evaluation at ER revealed a hypotensive patient that responded to initial resuscitation interventions. Examination showed a benign abdomen and digital rectal exam revealed no blood. Initial labs indicated a drop in hemoglobin to 8.7 g/dL (from a baseline of 11 g/dL), with stable platelet counts and normal renal and liver function. Patient was admitted and GI service consulted. EGD performed failed to identify a source of bleeding. Subsequently, capsule endoscopy was performed and showed a focus of active bleeding in the proximal duodenum. EGD was repeated confirming the presence of a dilated submucosal artery with active oozing in the second portion of the duodenum compatible with a Dieulafoy lesion. Hemostasis was achieved after injection of epinephrine, clip placement, and argon plasma coagulation. Post-treatment, the patient resumed apixaban with plan for left atrial appendage (LAA) closure for stroke prevention, allowing the discontinuation of anticoagulation without further bleeding.
Discussion: This case demonstrates the value of capsule endoscopy for detecting Dieulafoy lesions not identified on EGD. It also highlights the critical role of GI specialists in managing patients at high risk of life-threatening bleeding and the potential benefit of LAA closure for stroke prevention in those with atrial fibrillation.
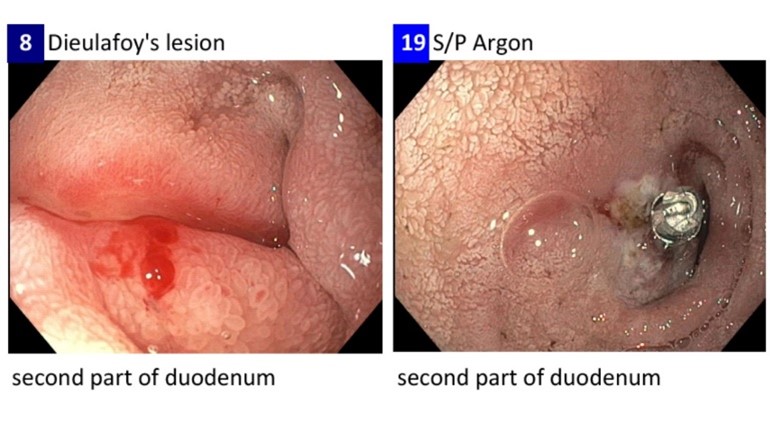
Figure: Left: EGD confirming a dilated submucosal artery with active oozing that was eroding the overlying mucosa of the second portion of duodenum compatible with a Dieulafoy lesion.
Right: Hemostasis achieved after injection of epinephrine, endoscopic clip placement, followed by argon plasma coagulation.
Right: Hemostasis achieved after injection of epinephrine, endoscopic clip placement, followed by argon plasma coagulation.
Disclosures:
Jesus Rivera-Rosa indicated no relevant financial relationships.
Reyshley Ramos-Márquez indicated no relevant financial relationships.
Roberto Rodriguez-Ramos indicated no relevant financial relationships.
Jose Martin-Ortiz indicated no relevant financial relationships.
Jesus Rivera-Rosa, MD1, Reyshley Ramos-Márquez, MD2, Roberto Rodriguez-Ramos, MD2, Jose Martin-Ortiz, MD, FACG2. P2473 - Revealing the Hidden Culprit: Dieulafoy Lesion as a Cause of Life-Threatening Gastrointestinal Bleeding in a Patient on Chronic Anticoagulation Therapy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
