Monday Poster Session
Category: Esophagus
P2245 - Opioid-Induced Esophageal Dysfunction Masquerading as Type I Achalasia
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Nicol Tugarinov, BS
University of Maryland School of Medicine
Baltimore, MD
Presenting Author(s)
Nicol Tugarinov, BS1, Andrew Leopold, MD, MS2, Guofeng Xie, MD, PhD2
1University of Maryland School of Medicine, Baltimore, MD; 2University of Maryland Medical Center, Baltimore, MD
Introduction: Opioid-induced esophageal dysfunction (OIED) is an esophageal motility disorder presenting as symptoms of dysphagia or chest pain with abnormal manometric testing and at least three months of continuous, daily opioid use. Manometric findings of type III achalasia, esophagogastric junction outflow obstruction, distal esophageal spasm, and hypercontractile esophagus have been commonly described in OIED. Recommended OIED management focused on opioid cessation prior to consideration of more invasive therapies.
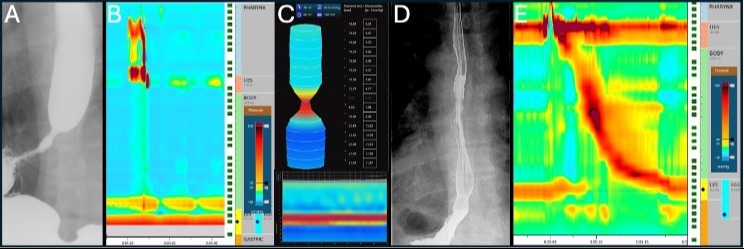
Case Description/Methods: A 49-year-old male with a history of opioid use disorder in remission on buprenorphine presented with solid and liquid dysphagia. Esophagogastroduodenoscopy (EGD) at symptom onset was normal. The patient re-presented four years later due to worsening dysphagia, with an Eckardt Score (ES) of 6. Barium esophagram (BE) showed a focal and fixed narrowing at the esophagogastric junction (EGJ) with stasis of contrast proximal to the narrowing (Figure 1A). High resolution esophageal manometry (HREM) showed a high resting lower esophageal sphincter (LES) pressure with absent peristalsis. Integrated relaxation pressure could not be quantified because the catheter did not traverse the LES. HREM suggested type I achalasia (Figure 1B). He was referred for confirmation of achalasia with endoluminal functional lumen imaging probe (EndoFLIP) and consideration for peroral endoscopic myotomy (POEM), with a simultaneous recommendation to decrease buprenorphine use through chronic pain management. EndoFLIP showed reduced EGJ opening with a weak contractile response, consistent with type I achalasia (Figure 1C). Four months after opioid taper initiation, ES was 2 and POEM was deferred due to symptomatic response to the buprenorphine taper. One month later, EGD with Botulinum toxin injection of the LES was performed with no clinical response by ES one month post-operatively. Six months after taper initiation, the patient ceased opioid use and ES was 0. Repeat BE demonstrated normal contrast emptying and repeat HREM was normal (Figure 1D-E).
Discussion: OIED is characterized by dysphagia and chest pain and is accompanied by heterogenous manometric findings in the setting of chronic opioid use. This novel case describes a patient with OIED masquerading, for the first time, as type I achalasia with complete symptom resolution and normalized manometric findings with cessation of opioid medication.
Disclosures:
Nicol Tugarinov, BS1, Andrew Leopold, MD, MS2, Guofeng Xie, MD, PhD2. P2245 - Opioid-Induced Esophageal Dysfunction Masquerading as Type I Achalasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Maryland School of Medicine, Baltimore, MD; 2University of Maryland Medical Center, Baltimore, MD
Introduction: Opioid-induced esophageal dysfunction (OIED) is an esophageal motility disorder presenting as symptoms of dysphagia or chest pain with abnormal manometric testing and at least three months of continuous, daily opioid use. Manometric findings of type III achalasia, esophagogastric junction outflow obstruction, distal esophageal spasm, and hypercontractile esophagus have been commonly described in OIED. Recommended OIED management focused on opioid cessation prior to consideration of more invasive therapies.
Case Description/Methods: A 49-year-old male with a history of opioid use disorder in remission on buprenorphine presented with solid and liquid dysphagia. Esophagogastroduodenoscopy (EGD) at symptom onset was normal. The patient re-presented four years later due to worsening dysphagia, with an Eckardt Score (ES) of 6. Barium esophagram (BE) showed a focal and fixed narrowing at the esophagogastric junction (EGJ) with stasis of contrast proximal to the narrowing (Figure 1A). High resolution esophageal manometry (HREM) showed a high resting lower esophageal sphincter (LES) pressure with absent peristalsis. Integrated relaxation pressure could not be quantified because the catheter did not traverse the LES. HREM suggested type I achalasia (Figure 1B). He was referred for confirmation of achalasia with endoluminal functional lumen imaging probe (EndoFLIP) and consideration for peroral endoscopic myotomy (POEM), with a simultaneous recommendation to decrease buprenorphine use through chronic pain management. EndoFLIP showed reduced EGJ opening with a weak contractile response, consistent with type I achalasia (Figure 1C). Four months after opioid taper initiation, ES was 2 and POEM was deferred due to symptomatic response to the buprenorphine taper. One month later, EGD with Botulinum toxin injection of the LES was performed with no clinical response by ES one month post-operatively. Six months after taper initiation, the patient ceased opioid use and ES was 0. Repeat BE demonstrated normal contrast emptying and repeat HREM was normal (Figure 1D-E).
Discussion: OIED is characterized by dysphagia and chest pain and is accompanied by heterogenous manometric findings in the setting of chronic opioid use. This novel case describes a patient with OIED masquerading, for the first time, as type I achalasia with complete symptom resolution and normalized manometric findings with cessation of opioid medication.
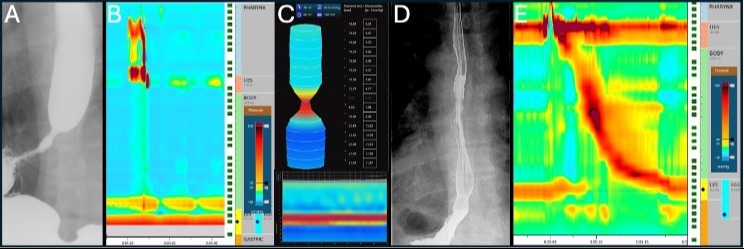
Figure: A-C are patient images associated with chronic opioid use. D and E demonstrate normalization of the patient studies with cessation of opioid medications. A) The BE shows a narrowing at the EGJ with delayed contrast emptying. B) HREM shows absent esophageal body peristalsis, and a suggestion of elevated LES pressures, which could not be quantified due to the inability of the HREM catheter to traverse the LES. C) EndoFLIP demonstrates a persistently elevated DI with a narrow diameter, with a classification of reduced EGJ opening and weak contractile response. D) After opioid medication cessation, the BE demonstrated normal emptying of contrast. E) After opioid cessation, the HREM normalized.
Disclosures:
Nicol Tugarinov indicated no relevant financial relationships.
Andrew Leopold indicated no relevant financial relationships.
Guofeng Xie indicated no relevant financial relationships.
Nicol Tugarinov, BS1, Andrew Leopold, MD, MS2, Guofeng Xie, MD, PhD2. P2245 - Opioid-Induced Esophageal Dysfunction Masquerading as Type I Achalasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

