Monday Poster Session
Category: Colon
P2086 - Eosinophilic Gastroenteritis and Colitis in a Patient With Concomitant Echinococcus Infection
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Talwinder Nagi, MD
Florida International University
Boca Raton, FL
Presenting Author(s)
Talwinder Nagi, MD1, Kathy N. Williams, MD, MS2, Jay Patel, MD3, Daniel Garrido, MD3, Adib Chaaya, MD4
1Florida International University, Boca Raton, FL; 2Cooper University Hospital, Philadelphia, PA; 3Cooper University Hospital, Camden, NJ; 4Cooper Health Gastroenterology, Camden, NJ
Introduction: Eosinophilic gastroenteritis (EG) and colitis (EC) results from infiltration of eosinophils in the mucosa, submucosa, or muscularis layer. It is a rare condition with a prevalence of 5.1 per 100,000 people. Risks include atopic diseases, autoimmune conditions like celiac disease, and parasitic infections. We present a case of a woman with no atopy who presented with GI symptoms and found to have biopsy proven EG and EC, along with concomitant Echinococcus infection.
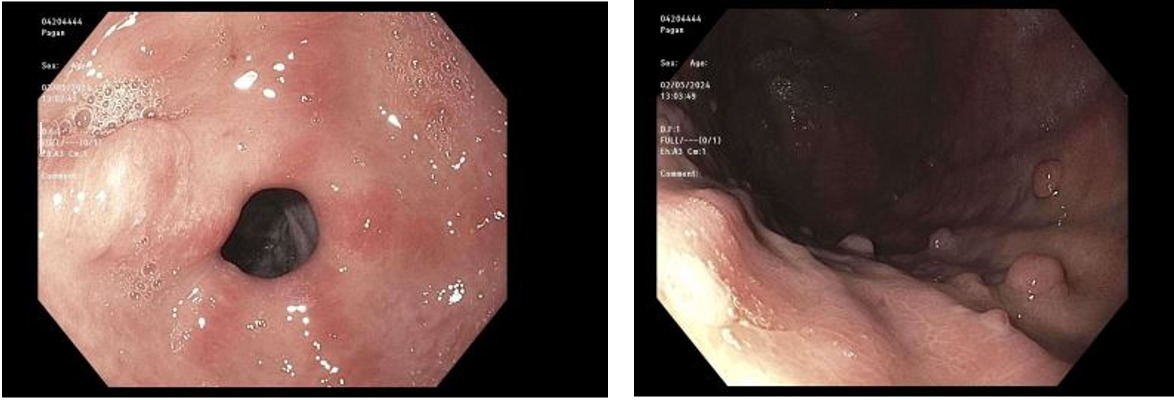
Case Description/Methods: 51-year-old woman with type I SOD post ERCP presented with abdominal pain and diarrhea. She denied travel, new foods, or recent antibiotics. She was overall stable and exam revealed epigastric pain and rectal with brown stool. Labs revealed WBC of 18.21, ALP 127, negative hepatitis panel and Clostridium difficile. A CTAP revealed pneumobilia, likely post-ERCP, and hepatic steatosis. She was managed supportively for viral gastroenteritis but had progressive vomiting and diarrhea. An EGD found erythematous mucosa in the antrum and gastric polyps. Colonoscopy found generalized erythematous mucosa. Pathology was negative for H.Pylori but found conspicuous eosinophils in the lamina propria of the antrum and duodenum, and increased eosinophils in the gastric polyp. Terminal ileum and ascending colon had eosinophilic cryptitis, and transverse and descending colon had increased eosinophils. Stool ova and parasites; Strongyloides, Coccidioides, ANA, RF, ANCAs, C3/4, and tryptase were negative. However, she had elevated IgE at 5980 and positive Echinococcus IgG. Ivermectin was started and a bone marrow biopsy found eosinophilia. Her abdominal pain and WBC normalized. An MRI of her liver was unremarkable, she established care with an allergist, and her eosinophilia was suspected due to the infectious cause.
Discussion:
EG and EC are complex disorders requiring a multidisciplinary approach for diagnosis and management. Hallmark features include elevated serum eosinophil counts and tissue biopsies. Management is based on suspected etiology but includes dietary modifications and pharmacotherapy with steroids. In our case, therapy with Ivermectin for Echinococcus may have led to improvement. In refractory cases, immunomodulators targeting eosinophil activity may be considered. Advances in understanding the immunologic and genetic factors are crucial for developing targeted therapies. Research should focus on diagnostic markers and therapeutic agents to improve the quality of life for affected individuals.
Disclosures:
Talwinder Nagi, MD1, Kathy N. Williams, MD, MS2, Jay Patel, MD3, Daniel Garrido, MD3, Adib Chaaya, MD4. P2086 - Eosinophilic Gastroenteritis and Colitis in a Patient With Concomitant Echinococcus Infection, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Florida International University, Boca Raton, FL; 2Cooper University Hospital, Philadelphia, PA; 3Cooper University Hospital, Camden, NJ; 4Cooper Health Gastroenterology, Camden, NJ
Introduction: Eosinophilic gastroenteritis (EG) and colitis (EC) results from infiltration of eosinophils in the mucosa, submucosa, or muscularis layer. It is a rare condition with a prevalence of 5.1 per 100,000 people. Risks include atopic diseases, autoimmune conditions like celiac disease, and parasitic infections. We present a case of a woman with no atopy who presented with GI symptoms and found to have biopsy proven EG and EC, along with concomitant Echinococcus infection.
Case Description/Methods: 51-year-old woman with type I SOD post ERCP presented with abdominal pain and diarrhea. She denied travel, new foods, or recent antibiotics. She was overall stable and exam revealed epigastric pain and rectal with brown stool. Labs revealed WBC of 18.21, ALP 127, negative hepatitis panel and Clostridium difficile. A CTAP revealed pneumobilia, likely post-ERCP, and hepatic steatosis. She was managed supportively for viral gastroenteritis but had progressive vomiting and diarrhea. An EGD found erythematous mucosa in the antrum and gastric polyps. Colonoscopy found generalized erythematous mucosa. Pathology was negative for H.Pylori but found conspicuous eosinophils in the lamina propria of the antrum and duodenum, and increased eosinophils in the gastric polyp. Terminal ileum and ascending colon had eosinophilic cryptitis, and transverse and descending colon had increased eosinophils. Stool ova and parasites; Strongyloides, Coccidioides, ANA, RF, ANCAs, C3/4, and tryptase were negative. However, she had elevated IgE at 5980 and positive Echinococcus IgG. Ivermectin was started and a bone marrow biopsy found eosinophilia. Her abdominal pain and WBC normalized. An MRI of her liver was unremarkable, she established care with an allergist, and her eosinophilia was suspected due to the infectious cause.
Discussion:
EG and EC are complex disorders requiring a multidisciplinary approach for diagnosis and management. Hallmark features include elevated serum eosinophil counts and tissue biopsies. Management is based on suspected etiology but includes dietary modifications and pharmacotherapy with steroids. In our case, therapy with Ivermectin for Echinococcus may have led to improvement. In refractory cases, immunomodulators targeting eosinophil activity may be considered. Advances in understanding the immunologic and genetic factors are crucial for developing targeted therapies. Research should focus on diagnostic markers and therapeutic agents to improve the quality of life for affected individuals.
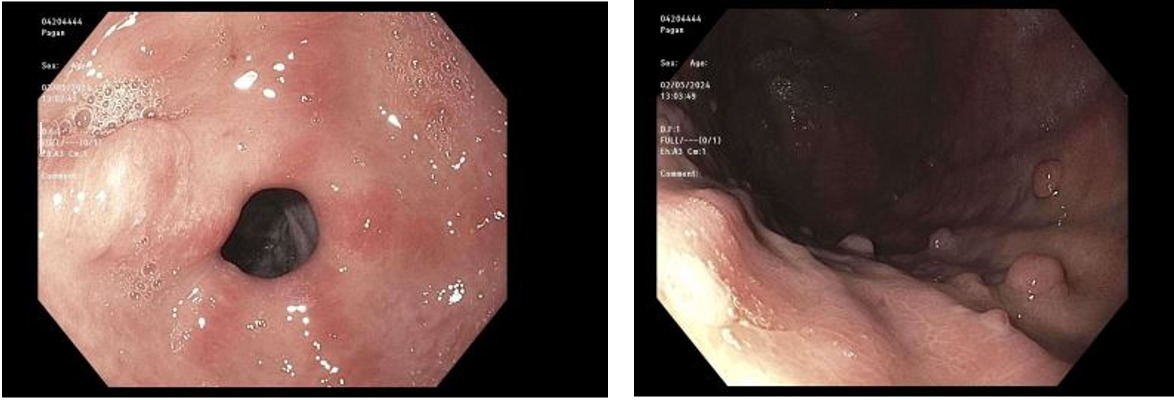
Figure: EGD with erythematous mucosa in the antrum and gastric polyps.
Disclosures:
Talwinder Nagi indicated no relevant financial relationships.
Kathy Williams indicated no relevant financial relationships.
Jay Patel indicated no relevant financial relationships.
Daniel Garrido indicated no relevant financial relationships.
Adib Chaaya indicated no relevant financial relationships.
Talwinder Nagi, MD1, Kathy N. Williams, MD, MS2, Jay Patel, MD3, Daniel Garrido, MD3, Adib Chaaya, MD4. P2086 - Eosinophilic Gastroenteritis and Colitis in a Patient With Concomitant Echinococcus Infection, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
