Monday Poster Session
Category: Colon
P2001 - Back to the Basics: Use Of Budesonide as the Treatment for Immune Checkpoint Inhibitor Induced Microscopic Colitis Non-Responsive to Prednisone, Infliximab, and Vedolizumab
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Zach Kovach, MD
West Virginia University
Morgantown, WV
Presenting Author(s)
Zach Kovach, MD1, Katherine Shepherd, MD1, Ethan M.. Cohen, MD1, Ayowumi Adekolu, MD1, Kanwarpreet Tandon, MD2
1West Virginia University, Morgantown, WV; 2West Virginia University School of Medicine, Morgantown, WV
Introduction: Immune checkpoint inhibitors (ICI) are highly effective monoclonal antibodies used in the treatment of various malignancies. However, development of immune-related adverse events (irAE) often precludes long-term treatment with these drugs. ICI colitis is a relatively common irAE characterized by profuse diarrhea, enterocolitis, and endoscopic and histological evidence of acute inflammation. In rare cases, ICI therapy can lead to the development of microscopic colitis (MC), a histologic diagnosis identified by lymphocytic infiltration in the colonic mucosa.
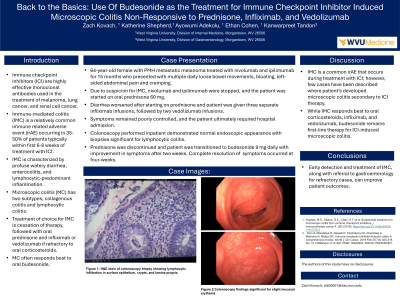
Case Description/Methods: A 64 year-old female with a past medical history of metastatic melanoma receiving ipilimumab and nivolumab therapy for 15 months presented with multiple daily loose bowel movements. There was associated bloating and occasional left-sided cramping, but she denied melena, hematochezia, or weight loss. An infectious workup for diarrhea was negative. Due to concern for immune mediated colitis (IMC) secondary to ICI, ipilimumab and nivolumab were stopped. The patient was started on prednisone at 60 mg daily dose per oncology with only partial improvement in symptoms. The diarrhea progressively worsened on prednisone taper and the patient was subsequently started on infliximab, for which she received three infusions with no improvement, followed by vedolizumab infusions x2 with similar results. The patient required hospitalization for her symptoms and gastroenterology was consulted. A colonoscopy was performed which showed normal endoscopic appearance of the colon and biopsies consistent with lymphocytic colitis. The prednisone was rapidly tapered off and patient was started on 9 mg budesonide daily to treat for MC. After transitioning to budesonide, the patient reported symptomatic improvement within 2 weeks and noted 1 formed bowel movement daily on 4-week outpatient follow up.
Discussion: ICI therapy is commonly associated with IMC, but rarely with MC. The management of these conditions differ, so we propose maintaining a broad differential for patients on ICI therapy who present with diarrhea and abdominal pain. IMC typically responds to corticosteroid therapy, infliximab and/or vedolizumab in refractory cases. However, budesonide remains first line therapy for ICI-induced microscopic colitis. Early gastroenterology consultation, endoscopic visualization, and histologic confirmation of diagnosis leads to appropriate identification and treatment of microscopic colitis, resulting in improved patient outcomes.
Disclosures:
Zach Kovach, MD1, Katherine Shepherd, MD1, Ethan M.. Cohen, MD1, Ayowumi Adekolu, MD1, Kanwarpreet Tandon, MD2. P2001 - Back to the Basics: Use Of Budesonide as the Treatment for Immune Checkpoint Inhibitor Induced Microscopic Colitis Non-Responsive to Prednisone, Infliximab, and Vedolizumab, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1West Virginia University, Morgantown, WV; 2West Virginia University School of Medicine, Morgantown, WV
Introduction: Immune checkpoint inhibitors (ICI) are highly effective monoclonal antibodies used in the treatment of various malignancies. However, development of immune-related adverse events (irAE) often precludes long-term treatment with these drugs. ICI colitis is a relatively common irAE characterized by profuse diarrhea, enterocolitis, and endoscopic and histological evidence of acute inflammation. In rare cases, ICI therapy can lead to the development of microscopic colitis (MC), a histologic diagnosis identified by lymphocytic infiltration in the colonic mucosa.
Case Description/Methods: A 64 year-old female with a past medical history of metastatic melanoma receiving ipilimumab and nivolumab therapy for 15 months presented with multiple daily loose bowel movements. There was associated bloating and occasional left-sided cramping, but she denied melena, hematochezia, or weight loss. An infectious workup for diarrhea was negative. Due to concern for immune mediated colitis (IMC) secondary to ICI, ipilimumab and nivolumab were stopped. The patient was started on prednisone at 60 mg daily dose per oncology with only partial improvement in symptoms. The diarrhea progressively worsened on prednisone taper and the patient was subsequently started on infliximab, for which she received three infusions with no improvement, followed by vedolizumab infusions x2 with similar results. The patient required hospitalization for her symptoms and gastroenterology was consulted. A colonoscopy was performed which showed normal endoscopic appearance of the colon and biopsies consistent with lymphocytic colitis. The prednisone was rapidly tapered off and patient was started on 9 mg budesonide daily to treat for MC. After transitioning to budesonide, the patient reported symptomatic improvement within 2 weeks and noted 1 formed bowel movement daily on 4-week outpatient follow up.
Discussion: ICI therapy is commonly associated with IMC, but rarely with MC. The management of these conditions differ, so we propose maintaining a broad differential for patients on ICI therapy who present with diarrhea and abdominal pain. IMC typically responds to corticosteroid therapy, infliximab and/or vedolizumab in refractory cases. However, budesonide remains first line therapy for ICI-induced microscopic colitis. Early gastroenterology consultation, endoscopic visualization, and histologic confirmation of diagnosis leads to appropriate identification and treatment of microscopic colitis, resulting in improved patient outcomes.
Disclosures:
Zach Kovach indicated no relevant financial relationships.
Katherine Shepherd indicated no relevant financial relationships.
Ethan Cohen indicated no relevant financial relationships.
Ayowumi Adekolu indicated no relevant financial relationships.
Kanwarpreet Tandon indicated no relevant financial relationships.
Zach Kovach, MD1, Katherine Shepherd, MD1, Ethan M.. Cohen, MD1, Ayowumi Adekolu, MD1, Kanwarpreet Tandon, MD2. P2001 - Back to the Basics: Use Of Budesonide as the Treatment for Immune Checkpoint Inhibitor Induced Microscopic Colitis Non-Responsive to Prednisone, Infliximab, and Vedolizumab, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
