Monday Poster Session
Category: Colon
P1924 - Colonic Stenting as a Bridge for Surgery and Palliative Approach: A Retrospective Review of Success and Complication
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Hussam Almasri, MD, MRCP
University of North Dakota
Fargo, ND
Presenting Author(s)
Hussam Almasri, MD, MRCP1, Bisher Sawaf, MD2, Kamran Mushtaq, MD3, Malik Halabya, MD3, Mhd Kutaiba Albuni, MD4, Mohammed Abderahim Hassan, MD3, Abdelatif Abdelmola, MD3, Saad Al Kaabi, MD3, Rafie Yakoob, MD3
1University of North Dakota, Fargo, ND; 2University of Toledo Health Sciences Campus, Toledo, OH; 3Hamad Medical Corporation, Doha, Ad Dawhah, Qatar; 4TriHealth, Doha, Ad Dawhah, Qatar
Introduction: The management of large bowel obstruction caused by colonic masses is shifting gradually from traditional emergency surgery to the use of self-expandable metal stents (SEMS) as a bridge for surgery. This approach is suggested to alleviate the obstruction and give more time for bowel relaxation before excisional surgery. In addition, using stents for acute colonic obstruction allows for careful tumor staging and planning for the best treatment. The other use of colonic stenting is for palliative management of colonic obstruction caused by advanced malignancies. This review highlights the success rate and complications associated with colonic stenting in the endoscopy center at Hamad Medical Corporation in Qatar.
Methods: Retrospective review comprising adult patients who underwent colonic stenting either for malignant-looking colonic obstruction before definite surgery or for symptomatic relief in metastatic non-operable cases between Jan 2015 and Dec 2022.
The baseline patient characteristics, type of stent, tumor stage, tumor site, stent complications, the need for colostomy, and stent failure data were collected using electronic medical records. Technical success was defined as the ability to properly deploy the stent. Clinical success was defined as the accomplishment of bowel evacuation and alleviation of the obstruction.
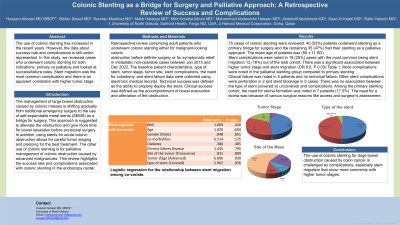
Results: 75 cases of colonic stenting were reviewed. 40 (53%) patients underwent stenting as a primary bridge for surgery and the remaining 35 (47%) had their stenting as a palliative approach. The mean age of patients was (55 ± 11 SD).
Stent complications were noted in 19 (25%) cases with the most common being stent migration 12 (16%) out of the total cohort. There was a significant association between higher tumor stage and stent migration (OR 6.8, P 0.03) Table 1. More complications were noted in the palliative stenting group compared to primary stenting
Clinical failure was noted in 5 patients and no technical failure. Other stent complications were perforation in 2 and stent blockage in 5 cases. There was no association between the type of stent (covered vs uncovered) and complications.
Among the primary stenting cohort, the need for stoma formation was noted in 7 patients (17.5%). The need for a stoma was because of various surgical reasons like access and surgeon's assessment.
Discussion: The use of colonic stenting for large bowel obstruction is challenged by complications, especially stent migration with higher tumor stages.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Hussam Almasri, MD, MRCP1, Bisher Sawaf, MD2, Kamran Mushtaq, MD3, Malik Halabya, MD3, Mhd Kutaiba Albuni, MD4, Mohammed Abderahim Hassan, MD3, Abdelatif Abdelmola, MD3, Saad Al Kaabi, MD3, Rafie Yakoob, MD3. P1924 - Colonic Stenting as a Bridge for Surgery and Palliative Approach: A Retrospective Review of Success and Complication, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of North Dakota, Fargo, ND; 2University of Toledo Health Sciences Campus, Toledo, OH; 3Hamad Medical Corporation, Doha, Ad Dawhah, Qatar; 4TriHealth, Doha, Ad Dawhah, Qatar
Introduction: The management of large bowel obstruction caused by colonic masses is shifting gradually from traditional emergency surgery to the use of self-expandable metal stents (SEMS) as a bridge for surgery. This approach is suggested to alleviate the obstruction and give more time for bowel relaxation before excisional surgery. In addition, using stents for acute colonic obstruction allows for careful tumor staging and planning for the best treatment. The other use of colonic stenting is for palliative management of colonic obstruction caused by advanced malignancies. This review highlights the success rate and complications associated with colonic stenting in the endoscopy center at Hamad Medical Corporation in Qatar.
Methods: Retrospective review comprising adult patients who underwent colonic stenting either for malignant-looking colonic obstruction before definite surgery or for symptomatic relief in metastatic non-operable cases between Jan 2015 and Dec 2022.
The baseline patient characteristics, type of stent, tumor stage, tumor site, stent complications, the need for colostomy, and stent failure data were collected using electronic medical records. Technical success was defined as the ability to properly deploy the stent. Clinical success was defined as the accomplishment of bowel evacuation and alleviation of the obstruction.
Results: 75 cases of colonic stenting were reviewed. 40 (53%) patients underwent stenting as a primary bridge for surgery and the remaining 35 (47%) had their stenting as a palliative approach. The mean age of patients was (55 ± 11 SD).
Stent complications were noted in 19 (25%) cases with the most common being stent migration 12 (16%) out of the total cohort. There was a significant association between higher tumor stage and stent migration (OR 6.8, P 0.03) Table 1. More complications were noted in the palliative stenting group compared to primary stenting
Clinical failure was noted in 5 patients and no technical failure. Other stent complications were perforation in 2 and stent blockage in 5 cases. There was no association between the type of stent (covered vs uncovered) and complications.
Among the primary stenting cohort, the need for stoma formation was noted in 7 patients (17.5%). The need for a stoma was because of various surgical reasons like access and surgeon's assessment.
Discussion: The use of colonic stenting for large bowel obstruction is challenged by complications, especially stent migration with higher tumor stages.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Hussam Almasri indicated no relevant financial relationships.
Bisher Sawaf indicated no relevant financial relationships.
Kamran Mushtaq indicated no relevant financial relationships.
Malik Halabya indicated no relevant financial relationships.
Mhd Kutaiba Albuni indicated no relevant financial relationships.
Mohammed Abderahim Hassan indicated no relevant financial relationships.
Abdelatif Abdelmola indicated no relevant financial relationships.
Saad Al Kaabi indicated no relevant financial relationships.
Rafie Yakoob indicated no relevant financial relationships.
Hussam Almasri, MD, MRCP1, Bisher Sawaf, MD2, Kamran Mushtaq, MD3, Malik Halabya, MD3, Mhd Kutaiba Albuni, MD4, Mohammed Abderahim Hassan, MD3, Abdelatif Abdelmola, MD3, Saad Al Kaabi, MD3, Rafie Yakoob, MD3. P1924 - Colonic Stenting as a Bridge for Surgery and Palliative Approach: A Retrospective Review of Success and Complication, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
