Monday Poster Session
Category: Colon
P1932 - Navigating Antithrombotic Medication Management for Colonoscopy: Patient Perspectives
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ria Minawala, MD
NYU Langone Health
New York, NY
Presenting Author(s)
Ria Minawala, MD1, Jessica H. Rauch, BS2, Seth Gross, MD1, Heiko Pohl, MD3, Aasma Shaukat, MD, MPH1
1NYU Langone Health, New York, NY; 2NYU Langone Health, Brooklyn, NY; 3Dartmouth Hitchcock Medical Center, White River Junction, VT
Introduction: A significant portion of patients undergoing colonoscopy with polypectomy are prescribed antithrombotic (AT) drugs, for cardiovascular or thromboembolic (TE) conditions. ATs increase the risk of post polypectomy bleeding (PPB), and guidelines recommend interruption of ATs prior to colonoscopy. However, there are currently no standardized, patient-centric guidelines on interruption and resumption timelines of ATs to mitigate the risk of PPB and TE events. Our aim was to conduct a qualitative, interview-based study to elucidate patient perspectives and concerns surrounding AT management for colonoscopy.
Methods: We identified patients in our healthcare system on ATs at the time of interview or past year, scheduled for or completed colonoscopy within the past year, and between 45-75 years of age and invited the first 11 eligible patients for interviews. Two independent reviewers coded and analyzed interview transcripts based on standard qualitative methods.
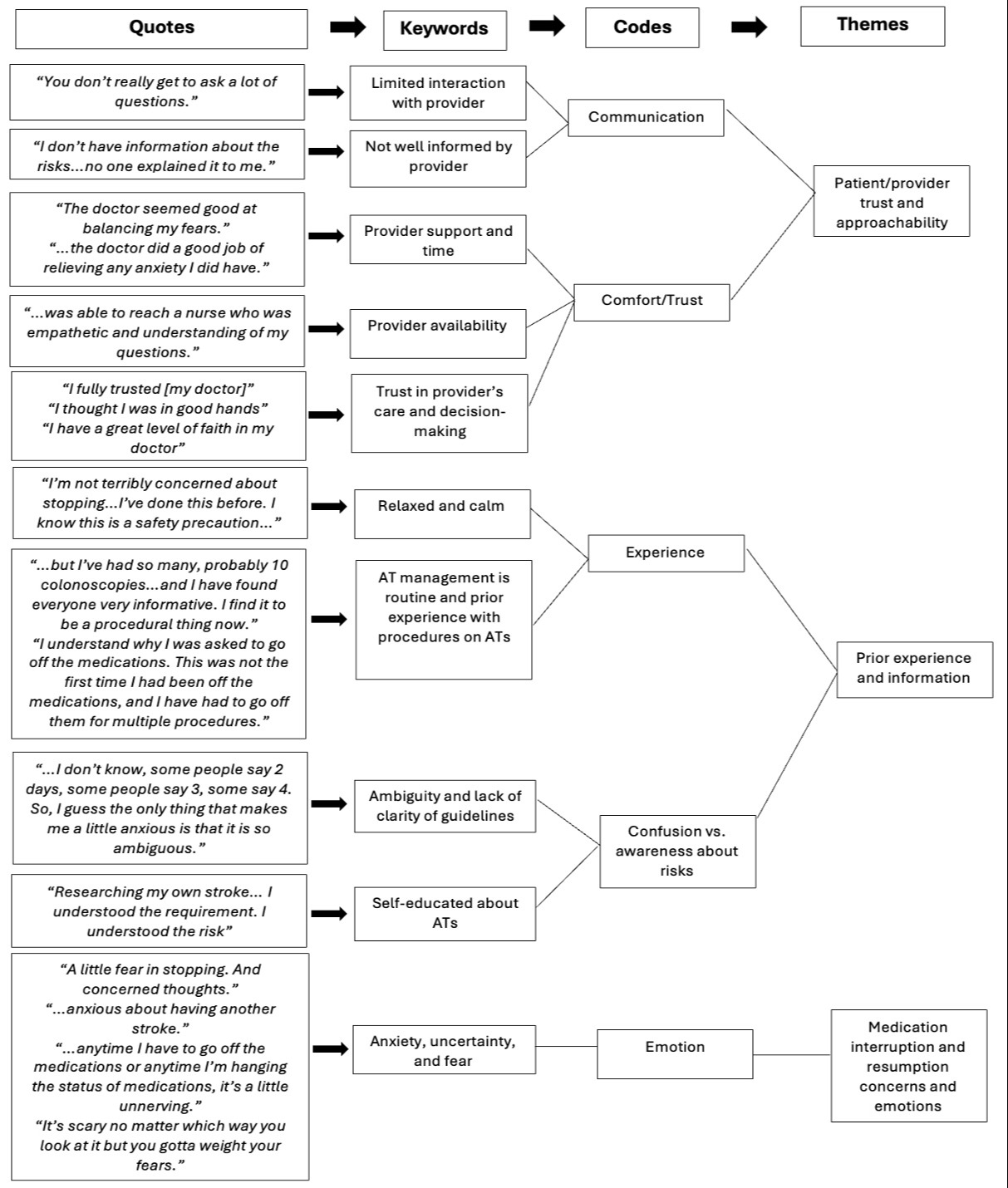
Results: In total, 11 patients were interviewed. The key themes we identified included provider trust/approachability, prior experience with AT interruption or prior colonoscopy, understanding of PPB/AT risks, prior experience discussing AT interruption/risks, mindsets about proceeding with colonoscopy, primary decision maker for AT management, and patient emotions. Six patients expressed feelings of concern and anxiety, including concern about TE events, PPB, and ambiguity regarding AT interruption and resumption timeline. The majority was more concerned about TE events than PPB. However, all six of these patients stated they would not delay or cancel future colonoscopy despite these feelings. Three patients reported lack of trust and approachability in their provider. All three voiced feelings of concern and/or anxiety over PPB. Of the eight patients who indicated prior experience with AT interruption for procedures, seven felt comfortable with approaching their healthcare team with questions. Additionally, all six patients who endorsed provider approachability expressed an understanding of AT interruption risks. (Figure 1)
Discussion: Trust and approachability of the provider was associated with feelings of anxiety about AT interruption. Given variability of AT management in clinical practice, discerning patient preferences and establishing trust can improve patient experiences and willingness to undergo colonoscopy. Our study highlights the importance of developing patient-centered protocols for clinical practice and future research.
Disclosures:
Ria Minawala, MD1, Jessica H. Rauch, BS2, Seth Gross, MD1, Heiko Pohl, MD3, Aasma Shaukat, MD, MPH1. P1932 - Navigating Antithrombotic Medication Management for Colonoscopy: Patient Perspectives, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1NYU Langone Health, New York, NY; 2NYU Langone Health, Brooklyn, NY; 3Dartmouth Hitchcock Medical Center, White River Junction, VT
Introduction: A significant portion of patients undergoing colonoscopy with polypectomy are prescribed antithrombotic (AT) drugs, for cardiovascular or thromboembolic (TE) conditions. ATs increase the risk of post polypectomy bleeding (PPB), and guidelines recommend interruption of ATs prior to colonoscopy. However, there are currently no standardized, patient-centric guidelines on interruption and resumption timelines of ATs to mitigate the risk of PPB and TE events. Our aim was to conduct a qualitative, interview-based study to elucidate patient perspectives and concerns surrounding AT management for colonoscopy.
Methods: We identified patients in our healthcare system on ATs at the time of interview or past year, scheduled for or completed colonoscopy within the past year, and between 45-75 years of age and invited the first 11 eligible patients for interviews. Two independent reviewers coded and analyzed interview transcripts based on standard qualitative methods.
Results: In total, 11 patients were interviewed. The key themes we identified included provider trust/approachability, prior experience with AT interruption or prior colonoscopy, understanding of PPB/AT risks, prior experience discussing AT interruption/risks, mindsets about proceeding with colonoscopy, primary decision maker for AT management, and patient emotions. Six patients expressed feelings of concern and anxiety, including concern about TE events, PPB, and ambiguity regarding AT interruption and resumption timeline. The majority was more concerned about TE events than PPB. However, all six of these patients stated they would not delay or cancel future colonoscopy despite these feelings. Three patients reported lack of trust and approachability in their provider. All three voiced feelings of concern and/or anxiety over PPB. Of the eight patients who indicated prior experience with AT interruption for procedures, seven felt comfortable with approaching their healthcare team with questions. Additionally, all six patients who endorsed provider approachability expressed an understanding of AT interruption risks. (Figure 1)
Discussion: Trust and approachability of the provider was associated with feelings of anxiety about AT interruption. Given variability of AT management in clinical practice, discerning patient preferences and establishing trust can improve patient experiences and willingness to undergo colonoscopy. Our study highlights the importance of developing patient-centered protocols for clinical practice and future research.
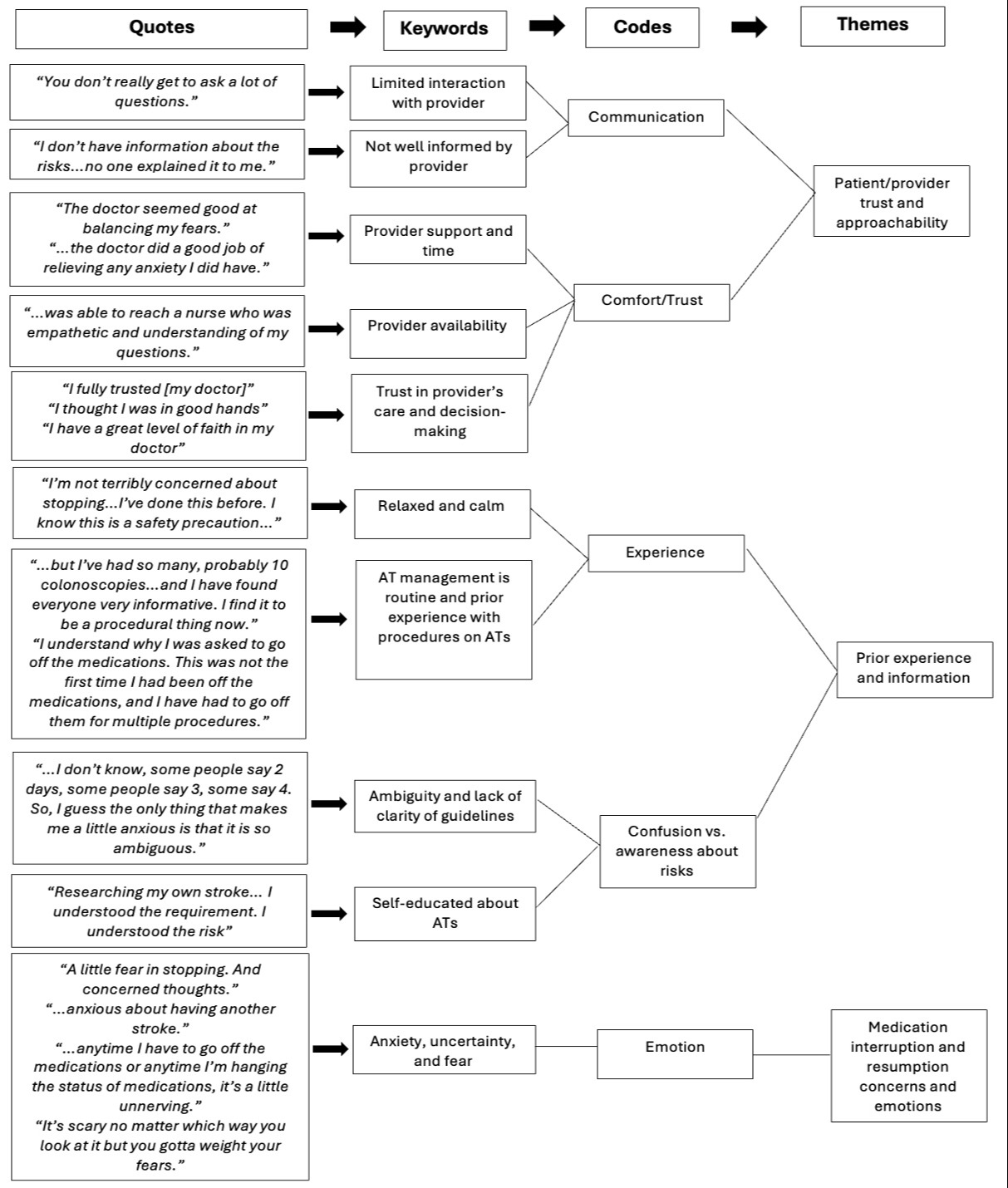
Figure: Figure 1. Example quotes and thematic analysis of interview transcripts using standard qualitative methods.
Abbreviations: AT, antithrombotic
Abbreviations: AT, antithrombotic
Disclosures:
Ria Minawala indicated no relevant financial relationships.
Jessica Rauch indicated no relevant financial relationships.
Seth Gross: Cook – Consultant. Medtronic – Consultant. Microtech – Consultant. Olympis – Consultant. Provation – Consultant.
Heiko Pohl: Cosmo – Grant/Research Support. InterVenn – Consultant. Pentax – Consultant. Steris – Grant/Research Support.
Aasma Shaukat: iterative health; Freenome – Consultant.
Ria Minawala, MD1, Jessica H. Rauch, BS2, Seth Gross, MD1, Heiko Pohl, MD3, Aasma Shaukat, MD, MPH1. P1932 - Navigating Antithrombotic Medication Management for Colonoscopy: Patient Perspectives, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

