Monday Poster Session
Category: Biliary/Pancreas
P1862 - The Problem to a Solution: A Case on Local Anesthetic-Related Acute Pancreatitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Jeffrey Robles, BS
CUNY School of Medicine and Northwell Health Staten Island University Hospital
Corona, NY
Presenting Author(s)
Jeffrey Robles, BS1, Dillon Rogando, BS2, Tara Ranjbar, MD3, Sourodip Mukharjee, MBBS4, Indraneil Mukherjee, MD4
1CUNY School of Medicine and Northwell Health Staten Island University Hospital, Corona, NY; 2CUNY School of Medicine and Northwell Health Staten Island University Hospital, Brooklyn, NY; 3Staten Island University Hospital, Northwell Health, Long Island, NY; 4Staten Island University Hospital, Northwell Health, Staten Island, NY
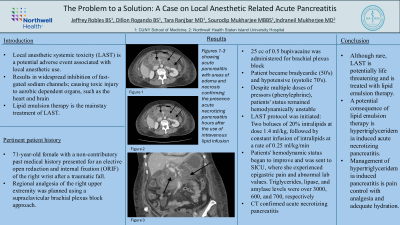
Introduction: Although rare, local anesthetic use has been associated with adverse central nervous system and cardiovascular adverse events. One complication is Local Anesthetic Systemic Toxicity, wherein the anesthetic agent inadvertently enters systemic circulation resulting in widespread inhibition of fast-gated sodium channels. Organs dependent on aerobic metabolism, such as the heart and brain, are especially susceptible to toxic injury resulting in cardiovascular collapse. Lipid emulsion therapy is a mainstay treatment of LAST, however, it may inadvertently cause lipid-induced necrotizing pancreatitis.
Case Description/Methods: 71-year-old female with a non-contributory past medical history who presented for elective ORIF of the right wrist after a fall onto the right hand one week prior. A supraclavicular brachial plexus block was planned to deliver regional analgesia for ORIF of the right wrist.
Discussion: Shortly after introduction of the local anesthetic agent, our patient became bradycardic and hypotensive. The patient's heart rate and systolic blood pressure remained in the low 45’s and 50s respectively, refractory to multiple doses of phenylephrine and ephedrine. Suspicion for LAST syndrome was high and lipid emulsion therapy was begun. Once stabilized, the patient was transported to the ICU requiring manual ventilation, where she later reported flank pain. Labs drawn were notable for elevated triglyceride, lipase, and amylase levels of over 3000, 600, and 700 respectively. CT imaging confirmed acute necrotizing pancreatitis.
Patients ICU stay was uncomplicated with stabilization of vitals and discharge 10 days later. Follow up with GI was scheduled for in two weeks. Since discharge, the patient noted intermittent abdominal aches. MRCP and MRI were performed after LFT’s were found to be elevated during her follow up appointment. MRI showed liquefaction necrosis of 80% of pancreas, with a 14 cm fluid collection pushing on the distal common bile duct, causing extrinsic obstruction. MRCP revealed no stones. Advanced GI placed a lumen apposing metal stent and drained the fluid from the obstructing cyst. Cytopathology came back as virtually acellular. Liver enzymes began to down trend appropriately and patient was discharged soon after. Follow-up at 2 and 4 days post-discharge confirmed resolution of symptoms.
Disclosures:
Jeffrey Robles, BS1, Dillon Rogando, BS2, Tara Ranjbar, MD3, Sourodip Mukharjee, MBBS4, Indraneil Mukherjee, MD4. P1862 - The Problem to a Solution: A Case on Local Anesthetic-Related Acute Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1CUNY School of Medicine and Northwell Health Staten Island University Hospital, Corona, NY; 2CUNY School of Medicine and Northwell Health Staten Island University Hospital, Brooklyn, NY; 3Staten Island University Hospital, Northwell Health, Long Island, NY; 4Staten Island University Hospital, Northwell Health, Staten Island, NY
Introduction: Although rare, local anesthetic use has been associated with adverse central nervous system and cardiovascular adverse events. One complication is Local Anesthetic Systemic Toxicity, wherein the anesthetic agent inadvertently enters systemic circulation resulting in widespread inhibition of fast-gated sodium channels. Organs dependent on aerobic metabolism, such as the heart and brain, are especially susceptible to toxic injury resulting in cardiovascular collapse. Lipid emulsion therapy is a mainstay treatment of LAST, however, it may inadvertently cause lipid-induced necrotizing pancreatitis.
Case Description/Methods: 71-year-old female with a non-contributory past medical history who presented for elective ORIF of the right wrist after a fall onto the right hand one week prior. A supraclavicular brachial plexus block was planned to deliver regional analgesia for ORIF of the right wrist.
Discussion: Shortly after introduction of the local anesthetic agent, our patient became bradycardic and hypotensive. The patient's heart rate and systolic blood pressure remained in the low 45’s and 50s respectively, refractory to multiple doses of phenylephrine and ephedrine. Suspicion for LAST syndrome was high and lipid emulsion therapy was begun. Once stabilized, the patient was transported to the ICU requiring manual ventilation, where she later reported flank pain. Labs drawn were notable for elevated triglyceride, lipase, and amylase levels of over 3000, 600, and 700 respectively. CT imaging confirmed acute necrotizing pancreatitis.
Patients ICU stay was uncomplicated with stabilization of vitals and discharge 10 days later. Follow up with GI was scheduled for in two weeks. Since discharge, the patient noted intermittent abdominal aches. MRCP and MRI were performed after LFT’s were found to be elevated during her follow up appointment. MRI showed liquefaction necrosis of 80% of pancreas, with a 14 cm fluid collection pushing on the distal common bile duct, causing extrinsic obstruction. MRCP revealed no stones. Advanced GI placed a lumen apposing metal stent and drained the fluid from the obstructing cyst. Cytopathology came back as virtually acellular. Liver enzymes began to down trend appropriately and patient was discharged soon after. Follow-up at 2 and 4 days post-discharge confirmed resolution of symptoms.
Disclosures:
Jeffrey Robles indicated no relevant financial relationships.
Dillon Rogando indicated no relevant financial relationships.
Tara Ranjbar indicated no relevant financial relationships.
Sourodip Mukharjee indicated no relevant financial relationships.
Indraneil Mukherjee indicated no relevant financial relationships.
Jeffrey Robles, BS1, Dillon Rogando, BS2, Tara Ranjbar, MD3, Sourodip Mukharjee, MBBS4, Indraneil Mukherjee, MD4. P1862 - The Problem to a Solution: A Case on Local Anesthetic-Related Acute Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
