Monday Poster Session
Category: Biliary/Pancreas
P1801 - Pancreatic Doppelgängers: A Case of Misdiagnosed Identity
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Aditya Kler, MD
University of Minnesota
Minneapolis, MN
Presenting Author(s)
Aditya Kler, MD1, Nirjhar Dutta, DO, MS2, Daniela Guerrero Vinsard, MD3
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN; 3University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: IGG-4 related disease (IgG4-RD) is an autoimmune condition that is difficult to diagnose and as many as 10% of cases may be misdiagnosed as pancreatic cancer initially.
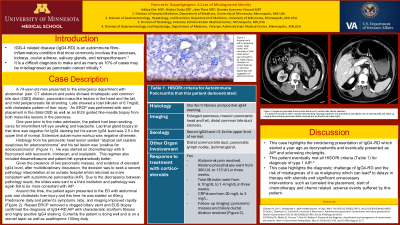
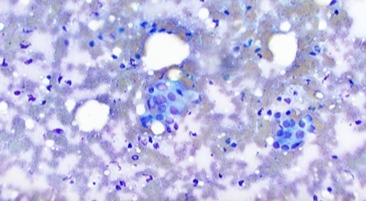
Case Description/Methods: A 74-year-old man presented to the ED with abdominal pain. CT abdomen and pelvis showed biliary dilation, pancreatic mass-like lesions in the head and the tail, and mild peripancreatic fat stranding. Labs showed a total bilirubin of 6.7mg/dL with cholestatic pattern of liver injury. An ERCP was performed with stent placement in the common bile and the pancreatic duct as well as an EUS guided fine-needle biopsy from both mass-like lesions in the pancreas. One year prior to the index admission, the patient had been seeking cares for intermittent left eye swelling and headache. Lacrimal gland biopsy at that time was negative for IgG4 staining but his serum IgG4 level was 2.5xULN. Extensive autoimmune workup was negative otherwise. Histology from his pancreatic head lesion yielded “atypical cell clusters suspicious for adenocarcinoma” and his tail lesion was “positive for adenocarcinoma” (Figure 1). He was started on chemotherapy with FOLFOXIRI, a regimen that also included dexamethasone and patient felt symptomatically better. Given the presence of two pancreatic masses, and evidence of elevated serum IgG4, a second pathology interpretation at another tertiary care center was sought and returned as equivocal for adenocarcinoma, continued to show atypical cells in a background of chronic pancreatitis and was rather suggestive of IgG4-RD. Due to the discrepancy between pathology reads, the slides were sent to a third institution and pathology was consistent with atypical changes most likely reactive in nature secondary to autoimmune pancreatitis. Around this time, the patient again presented to the ED with abdominal pain and cholestatic liver injury and this time he was started on 60mg prednisone daily and patient’s symptoms and labs improved rapidly. Repeat ERCP removed a clogged biliary stent but stent was not replaced. Repeat EUS biopsy confirmed the diagnosis of IgG4-RD AIP with characteristic storiform fibrosis and highly positive IgG4 staining. This patient eventually met all HISORt criteria (Table 1) for diagnosis of type 1 AIP. Currently the patient is doing well and is on a steroid taper as well as azathioprine 100mg daily.
Discussion: This case highlights the diagnostic challenge of IgG4-RD and the risk of misdiagnosis of it as malignancy.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Aditya Kler, MD1, Nirjhar Dutta, DO, MS2, Daniela Guerrero Vinsard, MD3. P1801 - Pancreatic Doppelgängers: A Case of Misdiagnosed Identity, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN; 3University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: IGG-4 related disease (IgG4-RD) is an autoimmune condition that is difficult to diagnose and as many as 10% of cases may be misdiagnosed as pancreatic cancer initially.
Case Description/Methods: A 74-year-old man presented to the ED with abdominal pain. CT abdomen and pelvis showed biliary dilation, pancreatic mass-like lesions in the head and the tail, and mild peripancreatic fat stranding. Labs showed a total bilirubin of 6.7mg/dL with cholestatic pattern of liver injury. An ERCP was performed with stent placement in the common bile and the pancreatic duct as well as an EUS guided fine-needle biopsy from both mass-like lesions in the pancreas. One year prior to the index admission, the patient had been seeking cares for intermittent left eye swelling and headache. Lacrimal gland biopsy at that time was negative for IgG4 staining but his serum IgG4 level was 2.5xULN. Extensive autoimmune workup was negative otherwise. Histology from his pancreatic head lesion yielded “atypical cell clusters suspicious for adenocarcinoma” and his tail lesion was “positive for adenocarcinoma” (Figure 1). He was started on chemotherapy with FOLFOXIRI, a regimen that also included dexamethasone and patient felt symptomatically better. Given the presence of two pancreatic masses, and evidence of elevated serum IgG4, a second pathology interpretation at another tertiary care center was sought and returned as equivocal for adenocarcinoma, continued to show atypical cells in a background of chronic pancreatitis and was rather suggestive of IgG4-RD. Due to the discrepancy between pathology reads, the slides were sent to a third institution and pathology was consistent with atypical changes most likely reactive in nature secondary to autoimmune pancreatitis. Around this time, the patient again presented to the ED with abdominal pain and cholestatic liver injury and this time he was started on 60mg prednisone daily and patient’s symptoms and labs improved rapidly. Repeat ERCP removed a clogged biliary stent but stent was not replaced. Repeat EUS biopsy confirmed the diagnosis of IgG4-RD AIP with characteristic storiform fibrosis and highly positive IgG4 staining. This patient eventually met all HISORt criteria (Table 1) for diagnosis of type 1 AIP. Currently the patient is doing well and is on a steroid taper as well as azathioprine 100mg daily.
Discussion: This case highlights the diagnostic challenge of IgG4-RD and the risk of misdiagnosis of it as malignancy.
Figure: Figure 1. Atypical cells with overlapping nuclei, large nuclei, and clumping of cells noted which were thought to be inflammatory changes; no mitotic features or abnormal appearing cells suggestive of adenocarcinoma.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Aditya Kler indicated no relevant financial relationships.
Nirjhar Dutta indicated no relevant financial relationships.
Daniela Guerrero Vinsard indicated no relevant financial relationships.
Aditya Kler, MD1, Nirjhar Dutta, DO, MS2, Daniela Guerrero Vinsard, MD3. P1801 - Pancreatic Doppelgängers: A Case of Misdiagnosed Identity, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
