Monday Poster Session
Category: Biliary/Pancreas
P1802 - An Uncommon Cause of Liver Abscess: Choledocholithiasis-Related Infection of Hepatic Cyst With Biliary Communication
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Stefan Thorarensen, MD, MPH
University of Connecticut Health
West Hartford, CT
Presenting Author(s)
Stefan Thorarensen, MD, MPH1, Rachael Hagen, DO2, Minh Thu T.. Nguyen, MD3, Murali Dharan, MD, MRCP3
1University of Connecticut Health, West Hartford, CT; 2University of Connecticut Health, Farmington, CT; 3University of Connecticut Health Center, Farmington, CT
Introduction: While rare, liver abscesses can be fatal, with mortality rates of 2-12%. Infections may stem from bacterial translocation, hematogenous spread, or the biliary tree. Here, we detail a recurring hepatic cyst identified as a pyogenic liver abscess (PLA) connected to the biliary duct.
Case Description/Methods: A 72-year-old woman with remote cholecystectomy and diverticulosis presented with weeks of generalized weakness and right upper quadrant abdominal pain. Her vital signs were normal. Initial lab work showed WBC (13.2 x10^3/uL), Hgb (12.3 g/dL), T-bili (0.4 mg/dL), ALT (9 IU/L), AST (12 IU/L), and alk phos (145 IU/L). Three years ago, she developed a 7.1 cm simple cyst in the left liver lobe, which grew to 10 cm within a few months. The cyst aspiration yielded 400 cc of yellow-green fluid, which was not analyzed.
During her hospitalization, she underwent ultrasound-guided drainage of a recurrent 9.5 cm liver cyst, which grew E. coli (Figure 1 & 2). Tests for ova and parasites, as well as echinococcus IgG, were negative. MRCP revealed common bile duct (CBD) dilation with two distal gallstones. Subsequent ERCP confirmed choledocholithiasis and moderate CBD dilation. A single cavity communicating with the left intra-hepatic biliary branches was identified, likely corresponding to the abscess cavity in the left liver lobe (Figure 3). Biliary sphincterotomy, balloon extraction, and a placement of a 7 Fr x 5 cm plastic CBD stent were performed. She clinically improved and was discharged with oral antibiotics (cefadroxil and metronidazole). Since her discharge four months ago, she has been doing well and is due for a follow-up ERCP.
Discussion: The presence of CBD dilation, gallstones, and a hepatic cavity communicating with the biliary tree, corresponding to the site of a previously drained cyst, strongly indicates biliary seeding as the origin of the abscess. PLAs pose a life-threatening risk of septic shock. Hepatic abscesses are rare, with an estimated incidence of 20 per 100,000 admissions, increasing with age and comorbidities such as diabetes and immunosuppression. Diagnostic tools include ultrasound, CT scan, MRCP, ERCP, and confirmation by needle aspiration. Treatment involves antibiotics, percutaneous drainage, and biliary drainage if a hepatobiliary connection is present. Literature on endoscopic management of hepatic cyst/abscess with biliary communication will be reviewed. This case underscores the importance of considering biliary communication for a recurrent hepatic cyst.

Disclosures:
Stefan Thorarensen, MD, MPH1, Rachael Hagen, DO2, Minh Thu T.. Nguyen, MD3, Murali Dharan, MD, MRCP3. P1802 - An Uncommon Cause of Liver Abscess: Choledocholithiasis-Related Infection of Hepatic Cyst With Biliary Communication, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Connecticut Health, West Hartford, CT; 2University of Connecticut Health, Farmington, CT; 3University of Connecticut Health Center, Farmington, CT
Introduction: While rare, liver abscesses can be fatal, with mortality rates of 2-12%. Infections may stem from bacterial translocation, hematogenous spread, or the biliary tree. Here, we detail a recurring hepatic cyst identified as a pyogenic liver abscess (PLA) connected to the biliary duct.
Case Description/Methods: A 72-year-old woman with remote cholecystectomy and diverticulosis presented with weeks of generalized weakness and right upper quadrant abdominal pain. Her vital signs were normal. Initial lab work showed WBC (13.2 x10^3/uL), Hgb (12.3 g/dL), T-bili (0.4 mg/dL), ALT (9 IU/L), AST (12 IU/L), and alk phos (145 IU/L). Three years ago, she developed a 7.1 cm simple cyst in the left liver lobe, which grew to 10 cm within a few months. The cyst aspiration yielded 400 cc of yellow-green fluid, which was not analyzed.
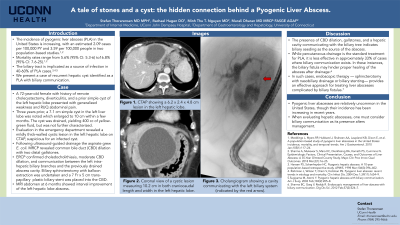
During her hospitalization, she underwent ultrasound-guided drainage of a recurrent 9.5 cm liver cyst, which grew E. coli (Figure 1 & 2). Tests for ova and parasites, as well as echinococcus IgG, were negative. MRCP revealed common bile duct (CBD) dilation with two distal gallstones. Subsequent ERCP confirmed choledocholithiasis and moderate CBD dilation. A single cavity communicating with the left intra-hepatic biliary branches was identified, likely corresponding to the abscess cavity in the left liver lobe (Figure 3). Biliary sphincterotomy, balloon extraction, and a placement of a 7 Fr x 5 cm plastic CBD stent were performed. She clinically improved and was discharged with oral antibiotics (cefadroxil and metronidazole). Since her discharge four months ago, she has been doing well and is due for a follow-up ERCP.
Discussion: The presence of CBD dilation, gallstones, and a hepatic cavity communicating with the biliary tree, corresponding to the site of a previously drained cyst, strongly indicates biliary seeding as the origin of the abscess. PLAs pose a life-threatening risk of septic shock. Hepatic abscesses are rare, with an estimated incidence of 20 per 100,000 admissions, increasing with age and comorbidities such as diabetes and immunosuppression. Diagnostic tools include ultrasound, CT scan, MRCP, ERCP, and confirmation by needle aspiration. Treatment involves antibiotics, percutaneous drainage, and biliary drainage if a hepatobiliary connection is present. Literature on endoscopic management of hepatic cyst/abscess with biliary communication will be reviewed. This case underscores the importance of considering biliary communication for a recurrent hepatic cyst.

Figure: Figure 1. An axial CT scan of the abdomen revealed a low-density lesion measuring 6.2 x 2.4 x 4.8 cm in the left hepatic lobe.
Figure 2. A coronal CT scan of the abdomen demonstrated a mildly thick-walled cystic lesion measuring 10.2 cm both craniocaudally and in width in the left hepatic lobe.
Figure 3. The cholangiogram showed a cavity communicating with the left biliary system (indicated by the red arrow).
Figure 2. A coronal CT scan of the abdomen demonstrated a mildly thick-walled cystic lesion measuring 10.2 cm both craniocaudally and in width in the left hepatic lobe.
Figure 3. The cholangiogram showed a cavity communicating with the left biliary system (indicated by the red arrow).
Disclosures:
Stefan Thorarensen indicated no relevant financial relationships.
Rachael Hagen indicated no relevant financial relationships.
Minh Thu Nguyen indicated no relevant financial relationships.
Murali Dharan indicated no relevant financial relationships.
Stefan Thorarensen, MD, MPH1, Rachael Hagen, DO2, Minh Thu T.. Nguyen, MD3, Murali Dharan, MD, MRCP3. P1802 - An Uncommon Cause of Liver Abscess: Choledocholithiasis-Related Infection of Hepatic Cyst With Biliary Communication, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
