Monday Poster Session
Category: Biliary/Pancreas
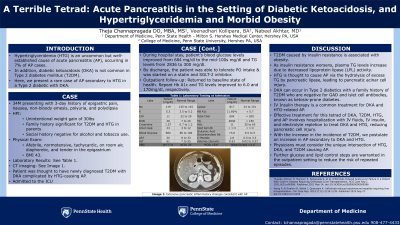
P1805 - A Terrible Tetrad: Acute Pancreatitis in the Setting of Diabetic Ketoacidosis, and Hypertriglyceridemia and Morbid Obesity
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Theja Channapragada, DO, MBA, MS
Penn State Health Milton S. Hershey Medical Center
Springfield, NJ
Presenting Author(s)
Theja Channapragada, DO, MBA, MS1, Veenadhari Kollipara, BA2, Nabeel Akhtar, MD2
1Penn State Health Milton S. Hershey Medical Center, Springfield, NJ; 2Penn State Health Milton S. Hershey Medical Center, Hershey, PA
Introduction: Hypertriglyceridemia (HTG) is an uncommon but well-established cause of acute pancreatitis (AP), occurring in 7% of AP cases. In addition, diabetic ketoacidosis (DKA) is not common in Type 2 diabetes mellitus (T2DM). Here, we present a rare case of AP secondary to HTG in a Type 2 diabetic with DKA.
Case Description/Methods: A 34-year-old male presented to the emergency department with a 3-day history of epigastric pain, nausea, non-bloody emesis, polyuria, and polydipsia. He reported unintentional weight gain of 30lbs. Family history is significant for T2DM and HTG in his parents. Social history negative for alcohol and tobacco use. On examination, the patient is afebrile, normotensive, tachycardic, on room air, diaphoretic, and tender in the epigastrium; BMI 43.
Laboratory testing is attached in Table 1. CT imaging showed extensive pancreatic inflammatory changes consistent with AP. The patient was thought to have newly diagnosed T2DM with DKA complicated by HTG-causing AP and was admitted to the intensive care unit. Management included Intravenous (IV) fluids, IV insulin drip, electrolyte replacement, bowel rest, and pain control. The patient’s blood glucose levels improved to the mid 100s mg/dl and TG levels to 300 mg/dl from admission to discharge. Before discharge, the patient was started on a statin and SGLT-2 inhibitor. He tolerated oral intake. Upon outpatient follow-up, he returned to his usual state of health, and repeat Hb A1c and TG improved to 6.0 and 170mg/dl, respectively.
Discussion: T2DM is caused by insulin resistance associated with obesity. As insulin resistance worsens, plasma TG levels increase due to decreased lipoprotein lipase (LPL) activity. HTG is thought to cause AP via the hydrolysis of excess TG by pancreatic lipase, leading to pancreatic acinar cell injury. DKA can occur in Type 2 diabetics with a family history of T2DM who are negative for GAD and islet cell antibodies, known as ketosis-prone diabetes.
IV Insulin therapy is a common treatment for DKA and HTG-related AP. Effective treatment for this tetrad of DKA, T2DM, HTG, and AP involves hospitalization with IV fluids, IV insulin, and electrolyte repletion to treat DKA and HTG, reducing pancreatic cell injury. With the increase in the incidence of T2DM, we postulate an increase in AP secondary to DKA and HTG. Physicians must consider the unique intersection of HTG, DKA, and T2DM causing AP. Further glucose and lipid control steps are warranted in the outpatient setting to reduce the risk of repeated episodes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Theja Channapragada, DO, MBA, MS1, Veenadhari Kollipara, BA2, Nabeel Akhtar, MD2. P1805 - A Terrible Tetrad: Acute Pancreatitis in the Setting of Diabetic Ketoacidosis, and Hypertriglyceridemia and Morbid Obesity, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Penn State Health Milton S. Hershey Medical Center, Springfield, NJ; 2Penn State Health Milton S. Hershey Medical Center, Hershey, PA
Introduction: Hypertriglyceridemia (HTG) is an uncommon but well-established cause of acute pancreatitis (AP), occurring in 7% of AP cases. In addition, diabetic ketoacidosis (DKA) is not common in Type 2 diabetes mellitus (T2DM). Here, we present a rare case of AP secondary to HTG in a Type 2 diabetic with DKA.
Case Description/Methods: A 34-year-old male presented to the emergency department with a 3-day history of epigastric pain, nausea, non-bloody emesis, polyuria, and polydipsia. He reported unintentional weight gain of 30lbs. Family history is significant for T2DM and HTG in his parents. Social history negative for alcohol and tobacco use. On examination, the patient is afebrile, normotensive, tachycardic, on room air, diaphoretic, and tender in the epigastrium; BMI 43.
Laboratory testing is attached in Table 1. CT imaging showed extensive pancreatic inflammatory changes consistent with AP. The patient was thought to have newly diagnosed T2DM with DKA complicated by HTG-causing AP and was admitted to the intensive care unit. Management included Intravenous (IV) fluids, IV insulin drip, electrolyte replacement, bowel rest, and pain control. The patient’s blood glucose levels improved to the mid 100s mg/dl and TG levels to 300 mg/dl from admission to discharge. Before discharge, the patient was started on a statin and SGLT-2 inhibitor. He tolerated oral intake. Upon outpatient follow-up, he returned to his usual state of health, and repeat Hb A1c and TG improved to 6.0 and 170mg/dl, respectively.
Discussion: T2DM is caused by insulin resistance associated with obesity. As insulin resistance worsens, plasma TG levels increase due to decreased lipoprotein lipase (LPL) activity. HTG is thought to cause AP via the hydrolysis of excess TG by pancreatic lipase, leading to pancreatic acinar cell injury. DKA can occur in Type 2 diabetics with a family history of T2DM who are negative for GAD and islet cell antibodies, known as ketosis-prone diabetes.
IV Insulin therapy is a common treatment for DKA and HTG-related AP. Effective treatment for this tetrad of DKA, T2DM, HTG, and AP involves hospitalization with IV fluids, IV insulin, and electrolyte repletion to treat DKA and HTG, reducing pancreatic cell injury. With the increase in the incidence of T2DM, we postulate an increase in AP secondary to DKA and HTG. Physicians must consider the unique intersection of HTG, DKA, and T2DM causing AP. Further glucose and lipid control steps are warranted in the outpatient setting to reduce the risk of repeated episodes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Theja Channapragada indicated no relevant financial relationships.
Veenadhari Kollipara indicated no relevant financial relationships.
Nabeel Akhtar indicated no relevant financial relationships.
Theja Channapragada, DO, MBA, MS1, Veenadhari Kollipara, BA2, Nabeel Akhtar, MD2. P1805 - A Terrible Tetrad: Acute Pancreatitis in the Setting of Diabetic Ketoacidosis, and Hypertriglyceridemia and Morbid Obesity, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
