Monday Poster Session
Category: Biliary/Pancreas
P1807 - A Rare Occurrence of Spontaneous Fistulization of Necrotizing Pancreatitis Into the Stomach and Duodenum
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Vera Hapshy, DO
Jersey Shore University Medical Center
Marlboro, NJ
Presenting Author(s)
Vera Hapshy, DO1, Harshavardan Sannekommu, MD2, Lauren Klei, MD2, Anne Marie Arcidiacono, DO2, Steven Imburgio, MD2, Swapnil Patel, MD2, Mohammad Hossain, MD2, Reza Akhtar, MD3, Lee Peng, MD, PhD3
1Jersey Shore University Medical Center, Marlboro, NJ; 2Jersey Shore University Medical Center, Neptune, NJ; 3Jersey Shore University Medical Center, Neptune City, NJ
Introduction: In necrotizing pancreatitis, patients can develop necrotic collections progressing to walled-off necrosis (WON) which seldom fistulizes. We present a unique case of acute pancreatitis complicated by pseudocysts with progression to necrotizing pancreatitis and formation of spontaneous pancreato-gastric and duodenal fistulas.
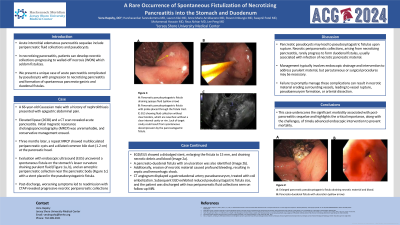
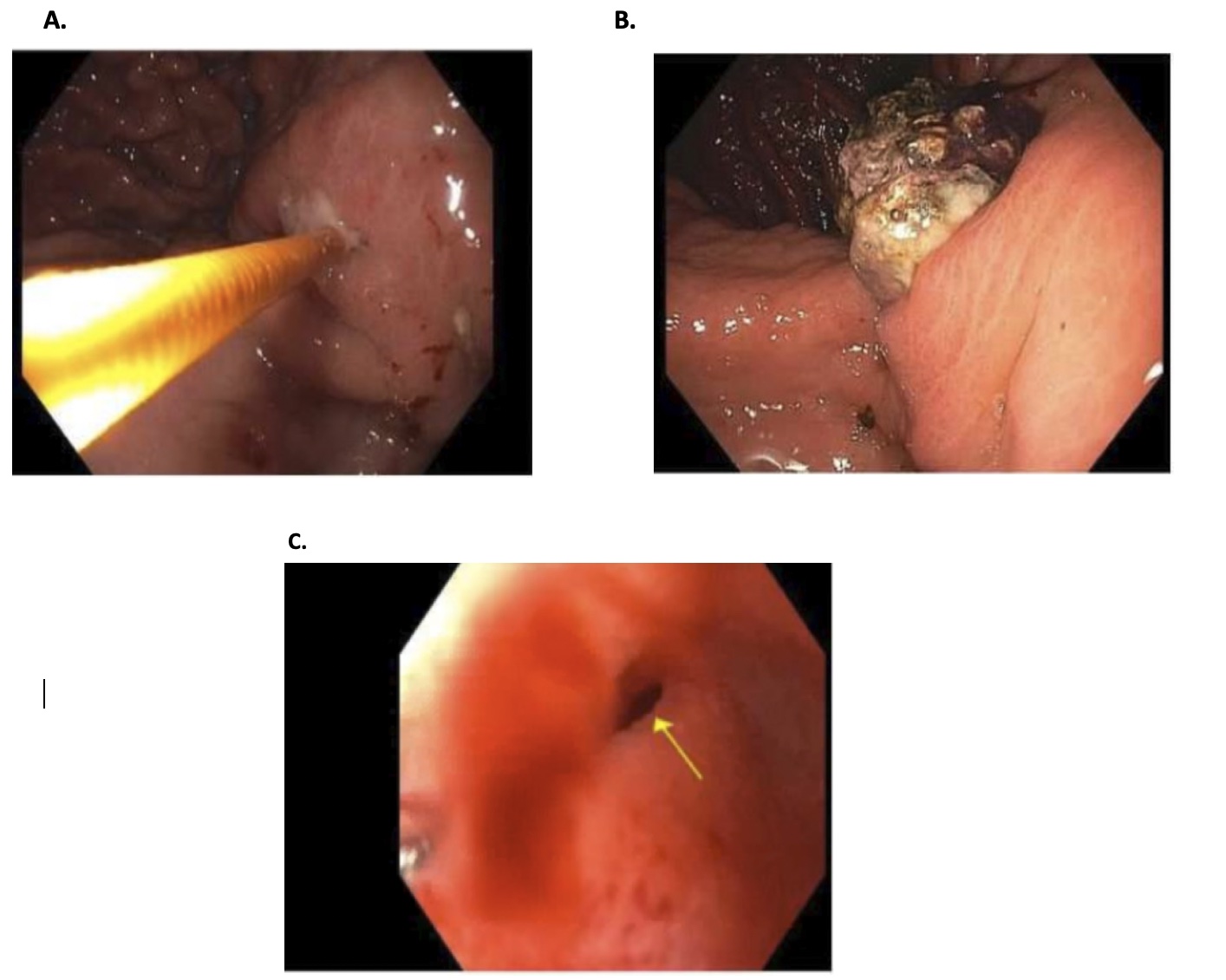
Case Description/Methods: A 66-year-old Caucasian male presented with epigastric abdominal pain. Elevated lipase (2638) and a CT scan revealed acute pancreatitis. Initial magnetic resonance cholangiopancreatography (MRCP) was unremarkable, and conservative management ensued. Three months later, a repeat MRCP showed multiloculated peripancreatic cysts and a dilated common bile duct (1.2 cm) at the pancreatic head. Evaluation with endoscopic ultrasound (EUS) uncovered a spontaneous fistula on the stomach's lesser curvature draining purulent fluid (Figure 1a), and an amorphic peripancreatic collection with a stent placed in the pseudocystogastric fistula. Post-discharge, worsening symptoms led to readmission. CTAP revealed progressive necrotic peripancreatic collections. EGD/EUS showed a dislodged stent, enlarging the fistula to 15mm, draining necrotic debris and blood (Figure 1b). A pancreato-duodenal fistula with an ulceration was also identified (Figure 1c). Additionally, erosion of necrotic material caused profound bleeding, resulting in septic and hemorrhagic shock. CT angiogram displayed a gastroduodenal artery pseudoaneurysm, treated with coil embolization. Subsequent EGD exhibited reduced pseudocystogastric fistula size, and the patient was discharged.
Discussion: Complications of pancreatitis, particularly in edematous and necrotizing forms, can be severe. Pancreatic pseudocysts may lead to pseudocystogastric fistulas upon rupture. Necrotic peripancreatic collections rarely progress to form duodenal fistulas usually associated with infection of necrotic pancreatic material. Management typically involves endoscopic drainage and intervention to address purulent material, but percutaneous or surgical procedures may be necessary. Failure to promptly manage these complications can result in necrotic material eroding surrounding vessels, leading to vessel rupture, pseudoaneurysm formation, or arterial dissection. This case underscores the significant morbidity associated with post-pancreatitis sequelae and highlights the importance and challenges of timely advanced endoscopic intervention to prevent mortality.
Disclosures:
Vera Hapshy, DO1, Harshavardan Sannekommu, MD2, Lauren Klei, MD2, Anne Marie Arcidiacono, DO2, Steven Imburgio, MD2, Swapnil Patel, MD2, Mohammad Hossain, MD2, Reza Akhtar, MD3, Lee Peng, MD, PhD3. P1807 - A Rare Occurrence of Spontaneous Fistulization of Necrotizing Pancreatitis Into the Stomach and Duodenum, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Jersey Shore University Medical Center, Marlboro, NJ; 2Jersey Shore University Medical Center, Neptune, NJ; 3Jersey Shore University Medical Center, Neptune City, NJ
Introduction: In necrotizing pancreatitis, patients can develop necrotic collections progressing to walled-off necrosis (WON) which seldom fistulizes. We present a unique case of acute pancreatitis complicated by pseudocysts with progression to necrotizing pancreatitis and formation of spontaneous pancreato-gastric and duodenal fistulas.
Case Description/Methods: A 66-year-old Caucasian male presented with epigastric abdominal pain. Elevated lipase (2638) and a CT scan revealed acute pancreatitis. Initial magnetic resonance cholangiopancreatography (MRCP) was unremarkable, and conservative management ensued. Three months later, a repeat MRCP showed multiloculated peripancreatic cysts and a dilated common bile duct (1.2 cm) at the pancreatic head. Evaluation with endoscopic ultrasound (EUS) uncovered a spontaneous fistula on the stomach's lesser curvature draining purulent fluid (Figure 1a), and an amorphic peripancreatic collection with a stent placed in the pseudocystogastric fistula. Post-discharge, worsening symptoms led to readmission. CTAP revealed progressive necrotic peripancreatic collections. EGD/EUS showed a dislodged stent, enlarging the fistula to 15mm, draining necrotic debris and blood (Figure 1b). A pancreato-duodenal fistula with an ulceration was also identified (Figure 1c). Additionally, erosion of necrotic material caused profound bleeding, resulting in septic and hemorrhagic shock. CT angiogram displayed a gastroduodenal artery pseudoaneurysm, treated with coil embolization. Subsequent EGD exhibited reduced pseudocystogastric fistula size, and the patient was discharged.
Discussion: Complications of pancreatitis, particularly in edematous and necrotizing forms, can be severe. Pancreatic pseudocysts may lead to pseudocystogastric fistulas upon rupture. Necrotic peripancreatic collections rarely progress to form duodenal fistulas usually associated with infection of necrotic pancreatic material. Management typically involves endoscopic drainage and intervention to address purulent material, but percutaneous or surgical procedures may be necessary. Failure to promptly manage these complications can result in necrotic material eroding surrounding vessels, leading to vessel rupture, pseudoaneurysm formation, or arterial dissection. This case underscores the significant morbidity associated with post-pancreatitis sequelae and highlights the importance and challenges of timely advanced endoscopic intervention to prevent mortality.
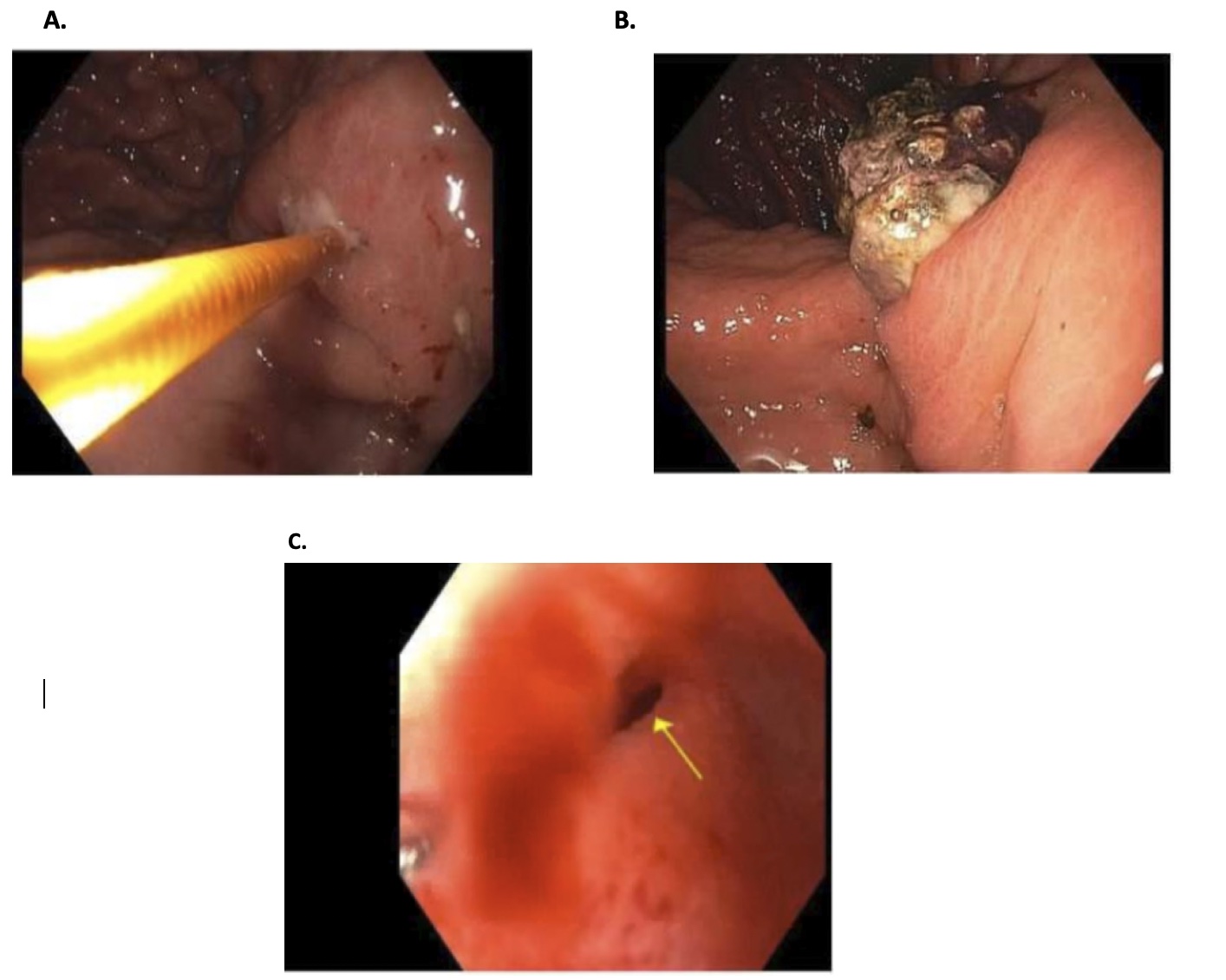
Figure: Figure 1
A: Pancreatic pseudocystogastric fistula with probe placed through the fistula tract draining opaque fluid
B: Enlarged pancreatic pseudocystogastric fistula draining necrotic material and blood.
C: Pancreato-duodenal fistula with ulceration (yellow arrow)
A: Pancreatic pseudocystogastric fistula with probe placed through the fistula tract draining opaque fluid
B: Enlarged pancreatic pseudocystogastric fistula draining necrotic material and blood.
C: Pancreato-duodenal fistula with ulceration (yellow arrow)
Disclosures:
Vera Hapshy indicated no relevant financial relationships.
Harshavardan Sannekommu indicated no relevant financial relationships.
Lauren Klei indicated no relevant financial relationships.
Anne Marie Arcidiacono indicated no relevant financial relationships.
Steven Imburgio indicated no relevant financial relationships.
Swapnil Patel indicated no relevant financial relationships.
Mohammad Hossain indicated no relevant financial relationships.
Reza Akhtar indicated no relevant financial relationships.
Lee Peng indicated no relevant financial relationships.
Vera Hapshy, DO1, Harshavardan Sannekommu, MD2, Lauren Klei, MD2, Anne Marie Arcidiacono, DO2, Steven Imburgio, MD2, Swapnil Patel, MD2, Mohammad Hossain, MD2, Reza Akhtar, MD3, Lee Peng, MD, PhD3. P1807 - A Rare Occurrence of Spontaneous Fistulization of Necrotizing Pancreatitis Into the Stomach and Duodenum, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
