Monday Poster Session
Category: Biliary/Pancreas
P1720 - A Comparative Analysis of Gender and Racial Disparities in Necrotizing Pancreatitis Outcomes: Insights From the National Inpatient Sample Database
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- NG
Niloy Ghosh, MD
University of New Mexico Health Sciences Center
Albuquerque, NM
Presenting Author(s)
Niloy Ghosh, MD, Abu Baker Sheikh, MD
University of New Mexico Health Sciences Center, Albuquerque, NM
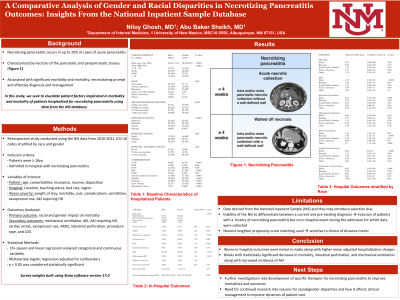
Introduction: Necrotizing pancreatitis occurs in up to 20% of cases of acute pancreatitis and is characterized by necrosis of the pancreatic and peripancreatic tissues. This is associated with significant morbidity and mortality, necessitating prompt and effective diagnosis and management. In this study, we seek to elucidate patient factors implicated in morbidity and mortality of patients hospitalized for necrotizing pancreatitis using data from the NIS database.
Methods: We utilized the United States NIS database to study clinical outcomes in hospitalized patients with necrotizing pancreatitis (a total of 118,580 patients) from 2018-2021. Propensity matching was conducted along with separate sub-group stratification by gender and race.
Results: From baseline characteristics, males were statically more likely to have CAD, DM, smoking history, and liver disease, while females were more likely to have chronic pulmonary disease, obesity, and metastatic cancer. Males were more likely to be put on mechanical ventilation (Adjusted odds ratio [aOR]: 1.35, P < 0.001), require vasopressors (aOR 1.26, P = 0.004), pass away in the hospital (aOR 1.14, P = 0.049), have an AKI requiring HD (aOR 1.54, P < 0.001), require surgical necrosectomy (aOR 1.45, P < 0.001), and have higher mean adjusted total hospitalization charges ($169,537 vs $152,718, P = 0.007).
Racial stratification utilized outcomes in Caucasians as the baseline comparison group. Blacks were found to have a statistically significant decrease in mortality (aOR 0.78, P = 0.02), intestinal perforation (aOR 0.33, P = 0.001), and mechanical ventilation (aOR 0.86, P = 0.03) along with higher incidence of AKI (aOR 1.19, P < 0.001) when compared to their Caucasian counterparts . No statistically significant difference was found between races regarding AKI requiring HD, vasopressor use, and ARDS.
Discussion: Worse in-hospital outcomes were noted in males along with higher mean adjusted hospitalization charges. In the racial stratification, Blacks were found to have a statistically significant decrease in mortality, intestinal perforation, and mechanical ventilation along with increased incidence of AKI. These results signify the need to prompt further investigations into the development of specific therapies for necrotizing pancreatitis in order to improve mortalities and outcomes, as further prospective studies analyzing patient factors and characteristics may help to enhance understandings of pathophysiology and subsequently improve dynamics of patient care.
Disclosures:
Niloy Ghosh, MD, Abu Baker Sheikh, MD. P1720 - A Comparative Analysis of Gender and Racial Disparities in Necrotizing Pancreatitis Outcomes: Insights From the National Inpatient Sample Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of New Mexico Health Sciences Center, Albuquerque, NM
Introduction: Necrotizing pancreatitis occurs in up to 20% of cases of acute pancreatitis and is characterized by necrosis of the pancreatic and peripancreatic tissues. This is associated with significant morbidity and mortality, necessitating prompt and effective diagnosis and management. In this study, we seek to elucidate patient factors implicated in morbidity and mortality of patients hospitalized for necrotizing pancreatitis using data from the NIS database.
Methods: We utilized the United States NIS database to study clinical outcomes in hospitalized patients with necrotizing pancreatitis (a total of 118,580 patients) from 2018-2021. Propensity matching was conducted along with separate sub-group stratification by gender and race.
Results: From baseline characteristics, males were statically more likely to have CAD, DM, smoking history, and liver disease, while females were more likely to have chronic pulmonary disease, obesity, and metastatic cancer. Males were more likely to be put on mechanical ventilation (Adjusted odds ratio [aOR]: 1.35, P < 0.001), require vasopressors (aOR 1.26, P = 0.004), pass away in the hospital (aOR 1.14, P = 0.049), have an AKI requiring HD (aOR 1.54, P < 0.001), require surgical necrosectomy (aOR 1.45, P < 0.001), and have higher mean adjusted total hospitalization charges ($169,537 vs $152,718, P = 0.007).
Racial stratification utilized outcomes in Caucasians as the baseline comparison group. Blacks were found to have a statistically significant decrease in mortality (aOR 0.78, P = 0.02), intestinal perforation (aOR 0.33, P = 0.001), and mechanical ventilation (aOR 0.86, P = 0.03) along with higher incidence of AKI (aOR 1.19, P < 0.001) when compared to their Caucasian counterparts . No statistically significant difference was found between races regarding AKI requiring HD, vasopressor use, and ARDS.
Discussion: Worse in-hospital outcomes were noted in males along with higher mean adjusted hospitalization charges. In the racial stratification, Blacks were found to have a statistically significant decrease in mortality, intestinal perforation, and mechanical ventilation along with increased incidence of AKI. These results signify the need to prompt further investigations into the development of specific therapies for necrotizing pancreatitis in order to improve mortalities and outcomes, as further prospective studies analyzing patient factors and characteristics may help to enhance understandings of pathophysiology and subsequently improve dynamics of patient care.
Disclosures:
Niloy Ghosh indicated no relevant financial relationships.
Abu Baker Sheikh indicated no relevant financial relationships.
Niloy Ghosh, MD, Abu Baker Sheikh, MD. P1720 - A Comparative Analysis of Gender and Racial Disparities in Necrotizing Pancreatitis Outcomes: Insights From the National Inpatient Sample Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
