Monday Poster Session
Category: Biliary/Pancreas
P1721 - Acute Pancreatitis in Pregnancy: Epidemiology and Treatment Outcomes
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- KH
Kathryn Hobbs, MD
Inova Fairfax Medical Campus
Fairfax, VA
Presenting Author(s)
Kathryn Hobbs, MD1, Dipam Shah, MD1, Reem Q.. Al Shabeeb, MD2, Marwan Abougergi, MD3
1Inova Fairfax Medical Campus, Fairfax, VA; 2Inova Fairfax Medical Campus, Silver Spring, MD; 3Inova Health System, Falls Church, PA
Introduction: Acute pancreatitis (AP) during pregnancy is a significant concern, posing risks to both maternal and fetal health. Most published research on this subject is based on small case series. In this study, we sought to determine the epidemiology, treatment modalities and outcomes of AP during pregnancy in the United States using the largest publicly available database.
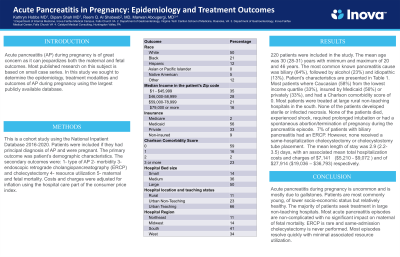
Methods: This is a cohort study using the National Inpatient Database 2016-2020. Patients were included if they had principal diagnosis of AP and were pregnant. The primary outcome was patient’s demographic characteristics. The secondary outcomes were: 1- type of AP 2- morbidity 4- endoscopic retrograde cholangiopancreatography (ERCP) and cholecystectomy 5- resource utilization 5- maternal and fetal mortality. Costs and charges were adjusted for inflation using the hospital care part of the consumer price index.
Results: 220 patients were included in the study. The mean age was 30 (28-31) years with minimum and maximum of 20 and 46 years. The most common known pancreatitis cause was biliary (64%), followed by alcohol (23%) and idiopathic (13%). Patient’s characteristics are presented in Table 1. Most patients where Caucasian (58%) from the lowest income quartile (33%), insured by Medicaid (56%) or privately (33%), and had a Charlson comorbidity score of 0. Most patients were treated at large rural non-teaching hospitals in the south. None of the patients developed sterile or infected necrosis. None of the patients died, experienced shock, required prolonged intubation or had a spontaneous abortion/termination of pregnancy during the pancreatitis episode. 7% of patients with biliary pancreatitis had an ERCP. However, none received a same-hospitalization cholecystectomy or cholecystostomy tube placement. The mean length of stay was 2.9 (2.2-3.5) days, with an associated mean total hospitalization costs and charges of $7,141 ($5,210 - $9,072) and of $27,914 ($19,036 – $36,793) respectively.
Discussion: Acute pancreatitis during pregnancy is uncommon and predominantly caused by gallstones. Affected patients are typically young, of lower socio-economic status but otherwise relatively healthy. Most seek treatment at large non-teaching hospitals. The majority of acute pancreatitis episodes are uncomplicated and do not significantly impact maternal or fetal mortality. ERCP is rarely performed and same-admission cholecystectomy is never conducted. Most episodes resolve quickly with minimal resource utilization
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kathryn Hobbs, MD1, Dipam Shah, MD1, Reem Q.. Al Shabeeb, MD2, Marwan Abougergi, MD3. P1721 - Acute Pancreatitis in Pregnancy: Epidemiology and Treatment Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Inova Fairfax Medical Campus, Fairfax, VA; 2Inova Fairfax Medical Campus, Silver Spring, MD; 3Inova Health System, Falls Church, PA
Introduction: Acute pancreatitis (AP) during pregnancy is a significant concern, posing risks to both maternal and fetal health. Most published research on this subject is based on small case series. In this study, we sought to determine the epidemiology, treatment modalities and outcomes of AP during pregnancy in the United States using the largest publicly available database.
Methods: This is a cohort study using the National Inpatient Database 2016-2020. Patients were included if they had principal diagnosis of AP and were pregnant. The primary outcome was patient’s demographic characteristics. The secondary outcomes were: 1- type of AP 2- morbidity 4- endoscopic retrograde cholangiopancreatography (ERCP) and cholecystectomy 5- resource utilization 5- maternal and fetal mortality. Costs and charges were adjusted for inflation using the hospital care part of the consumer price index.
Results: 220 patients were included in the study. The mean age was 30 (28-31) years with minimum and maximum of 20 and 46 years. The most common known pancreatitis cause was biliary (64%), followed by alcohol (23%) and idiopathic (13%). Patient’s characteristics are presented in Table 1. Most patients where Caucasian (58%) from the lowest income quartile (33%), insured by Medicaid (56%) or privately (33%), and had a Charlson comorbidity score of 0. Most patients were treated at large rural non-teaching hospitals in the south. None of the patients developed sterile or infected necrosis. None of the patients died, experienced shock, required prolonged intubation or had a spontaneous abortion/termination of pregnancy during the pancreatitis episode. 7% of patients with biliary pancreatitis had an ERCP. However, none received a same-hospitalization cholecystectomy or cholecystostomy tube placement. The mean length of stay was 2.9 (2.2-3.5) days, with an associated mean total hospitalization costs and charges of $7,141 ($5,210 - $9,072) and of $27,914 ($19,036 – $36,793) respectively.
Discussion: Acute pancreatitis during pregnancy is uncommon and predominantly caused by gallstones. Affected patients are typically young, of lower socio-economic status but otherwise relatively healthy. Most seek treatment at large non-teaching hospitals. The majority of acute pancreatitis episodes are uncomplicated and do not significantly impact maternal or fetal mortality. ERCP is rarely performed and same-admission cholecystectomy is never conducted. Most episodes resolve quickly with minimal resource utilization
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kathryn Hobbs indicated no relevant financial relationships.
Dipam Shah indicated no relevant financial relationships.
Reem Al Shabeeb indicated no relevant financial relationships.
Marwan Abougergi indicated no relevant financial relationships.
Kathryn Hobbs, MD1, Dipam Shah, MD1, Reem Q.. Al Shabeeb, MD2, Marwan Abougergi, MD3. P1721 - Acute Pancreatitis in Pregnancy: Epidemiology and Treatment Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
