Sunday Poster Session
Category: Biliary/Pancreas
P0034 - Predictive Yield of Targeted Endoscopic Ultrasound-Guided - Fine Needle Aspiration in Diagnosing Incidental Pancreatic Cysts
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- PG
Priyatham Gurram, MD
Central Michigan University College of Medicine
Saginaw, MI
Presenting Author(s)
Priyatham Gurram, MD1, Adil Mohammed, MD1, Joseph Hentz, 2, Longwen Chen, MD, PhD2, Michelle Ann. Anderson, MD, MSc3, Douglas Faigel, MD2, Norio Fukami, MD4, Cuong Nguyen, MD2, Rahul Pannala, MD3, Terry Jue, MD3
1Central Michigan University College of Medicine, Saginaw, MI; 2Mayo Clinic College of Medicine and Science, Scottsdale, AZ; 3Mayo Clinic, Scottsdale, AZ; 4Mayo Clinic, Phoenix, AZ
Introduction: Most incidental pancreatic cysts are benign. Many have malignant potential,
but few progress to cancer. Endoscopic ultrasound is recommended when cysts have
worrisome or high risk features on imaging, but when and how to perform EUS-guided fine
needle aspirate or biopsy (EUS-FNA/FNB) for tissue is unclear. Our study aims to determine
the diagnostic yield of EUS-FNA and determine if targeting cyst features for tissue provides
additional clinical value.
Methods: We conducted a retrospective analysis of 1411 patients with incidental pancreatic
cysts who underwent EUS-FNA from 2012 to 2022 at Mayo Clinic. Patients were
categorized as “Targeted” or “Not Targeted” FNA. Targeted was defined as tissue taken
when the needle was directed into a cyst wall, septae, mural nodule, or mass; and Not
Targeted was when cyst fluid aspirate was sent for cytology. Age, cyst characteristics,
cytological findings, and surgical pathology were compared. The predictive yield was when
pathology reported high-grade dysplasia(HGD), carcinoma, neuroendocrine tumor(NET),
serous cystadenoma, or metastatic cancer.
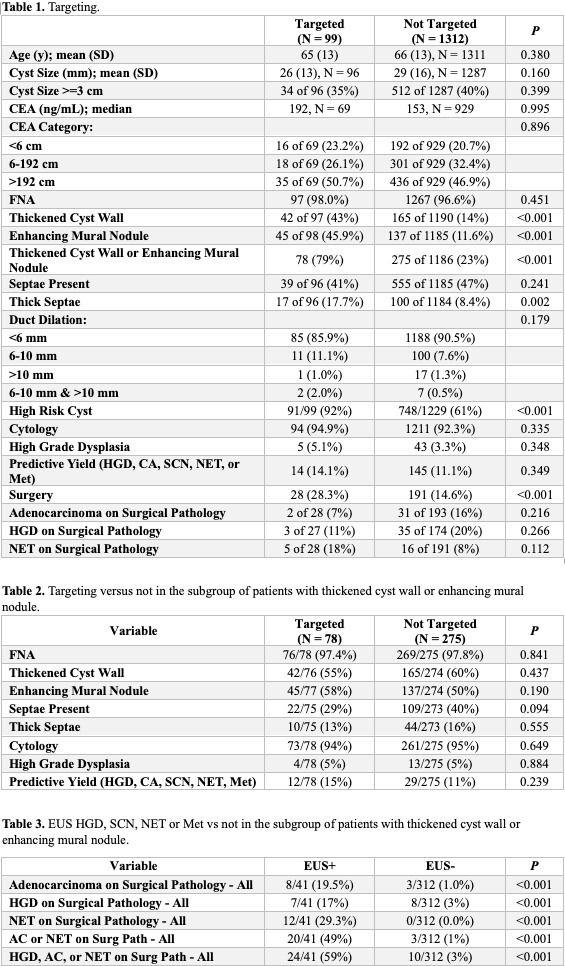
Results: Of 1411 patients, 99 were Targeted and 1312 Not targeted. There were no
significant differences in age, cyst size, or pancreatic duct dilation. Thickened cyst walls
(43% vs. 14% p< 0.001), enhancing mural nodules (45.9% vs.11.6% p< 0.001), and thick
septae (17.7% vs. 8.4% p=0.002) were more prevalent in the Targeted group. HGD was in
5.1% of the Targeted and 3.3% of the Not targeted groups(p=0.348). The Targeted group
had a higher rate of surgery (p< 0.001) but no significant difference in the incidence of
carcinoma or HGD on surgical pathology. As confirmed by surgical pathology, EUS-FNA
with HGD, carcinoma, or NET was predictive versus EUS-FNA without yield (59% vs. 3%
p< 0.001). But there was no significant difference in predictive yield with Targeted versus Not
targeted FNA(15% vs. 11% p=0.239).
Discussion: EUS-FNA should be performed in the setting of a mural nodule or thickened
septae or cyst wall as a positive result is predictive of HGD, NET or carcinoma. However,
Targeted EUS-FNA had no difference in predictive yield. While targeting the cyst features of
a complex pancreatic cyst during EUS-FNA is reasonable, discerning high risk features
remains essential in assessing malignant potential and should guide clinical decisions.
Patients whose cysts do not have high risk features may not benefit from EUS-FNA for
tissue. Our conclusions are limited by retrospective data.
Disclosures:
Priyatham Gurram, MD1, Adil Mohammed, MD1, Joseph Hentz, 2, Longwen Chen, MD, PhD2, Michelle Ann. Anderson, MD, MSc3, Douglas Faigel, MD2, Norio Fukami, MD4, Cuong Nguyen, MD2, Rahul Pannala, MD3, Terry Jue, MD3. P0034 - Predictive Yield of Targeted Endoscopic Ultrasound-Guided - Fine Needle Aspiration in Diagnosing Incidental Pancreatic Cysts, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Central Michigan University College of Medicine, Saginaw, MI; 2Mayo Clinic College of Medicine and Science, Scottsdale, AZ; 3Mayo Clinic, Scottsdale, AZ; 4Mayo Clinic, Phoenix, AZ
Introduction: Most incidental pancreatic cysts are benign. Many have malignant potential,
but few progress to cancer. Endoscopic ultrasound is recommended when cysts have
worrisome or high risk features on imaging, but when and how to perform EUS-guided fine
needle aspirate or biopsy (EUS-FNA/FNB) for tissue is unclear. Our study aims to determine
the diagnostic yield of EUS-FNA and determine if targeting cyst features for tissue provides
additional clinical value.
Methods: We conducted a retrospective analysis of 1411 patients with incidental pancreatic
cysts who underwent EUS-FNA from 2012 to 2022 at Mayo Clinic. Patients were
categorized as “Targeted” or “Not Targeted” FNA. Targeted was defined as tissue taken
when the needle was directed into a cyst wall, septae, mural nodule, or mass; and Not
Targeted was when cyst fluid aspirate was sent for cytology. Age, cyst characteristics,
cytological findings, and surgical pathology were compared. The predictive yield was when
pathology reported high-grade dysplasia(HGD), carcinoma, neuroendocrine tumor(NET),
serous cystadenoma, or metastatic cancer.
Results: Of 1411 patients, 99 were Targeted and 1312 Not targeted. There were no
significant differences in age, cyst size, or pancreatic duct dilation. Thickened cyst walls
(43% vs. 14% p< 0.001), enhancing mural nodules (45.9% vs.11.6% p< 0.001), and thick
septae (17.7% vs. 8.4% p=0.002) were more prevalent in the Targeted group. HGD was in
5.1% of the Targeted and 3.3% of the Not targeted groups(p=0.348). The Targeted group
had a higher rate of surgery (p< 0.001) but no significant difference in the incidence of
carcinoma or HGD on surgical pathology. As confirmed by surgical pathology, EUS-FNA
with HGD, carcinoma, or NET was predictive versus EUS-FNA without yield (59% vs. 3%
p< 0.001). But there was no significant difference in predictive yield with Targeted versus Not
targeted FNA(15% vs. 11% p=0.239).
Discussion: EUS-FNA should be performed in the setting of a mural nodule or thickened
septae or cyst wall as a positive result is predictive of HGD, NET or carcinoma. However,
Targeted EUS-FNA had no difference in predictive yield. While targeting the cyst features of
a complex pancreatic cyst during EUS-FNA is reasonable, discerning high risk features
remains essential in assessing malignant potential and should guide clinical decisions.
Patients whose cysts do not have high risk features may not benefit from EUS-FNA for
tissue. Our conclusions are limited by retrospective data.
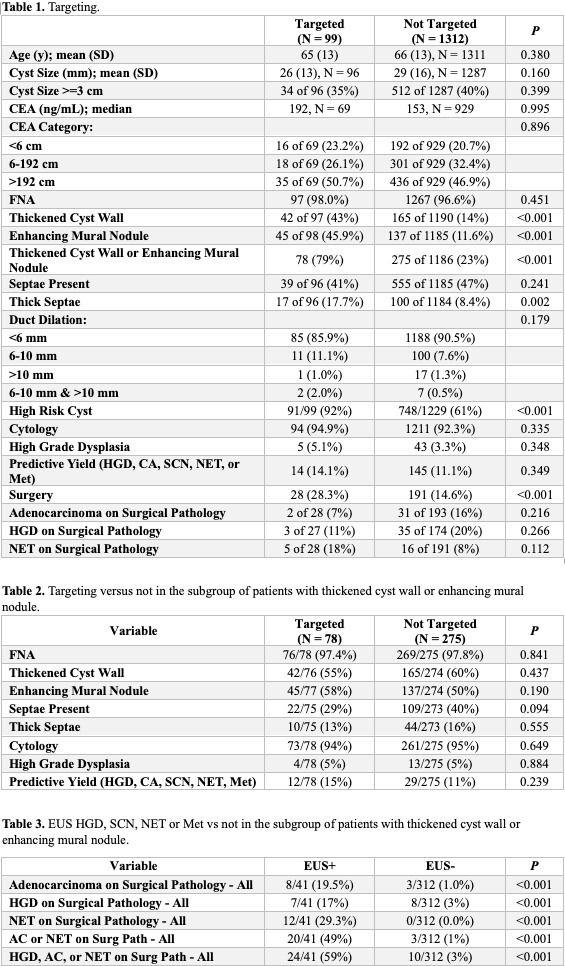
Figure: Comparision of outcomes in Targeting vs Not targeting the pancreatic cysts during EUS-FNA
Disclosures:
Priyatham Gurram indicated no relevant financial relationships.
Adil Mohammed indicated no relevant financial relationships.
Joseph Hentz indicated no relevant financial relationships.
Longwen Chen indicated no relevant financial relationships.
Michelle Anderson: Boston Scientific – Consultant.
Douglas Faigel indicated no relevant financial relationships.
Norio Fukami indicated no relevant financial relationships.
Cuong Nguyen indicated no relevant financial relationships.
Rahul Pannala: HCL Technologies – Consultant. Nestle Healthsciences – Advisor or Review Panel Member.
Terry Jue: Boston Scientific – Instructor.
Priyatham Gurram, MD1, Adil Mohammed, MD1, Joseph Hentz, 2, Longwen Chen, MD, PhD2, Michelle Ann. Anderson, MD, MSc3, Douglas Faigel, MD2, Norio Fukami, MD4, Cuong Nguyen, MD2, Rahul Pannala, MD3, Terry Jue, MD3. P0034 - Predictive Yield of Targeted Endoscopic Ultrasound-Guided - Fine Needle Aspiration in Diagnosing Incidental Pancreatic Cysts, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
