Sunday Poster Session
Category: Biliary/Pancreas
P0035 - Revealing Reality: National Readmissions Database Uncovers Higher Post-ERCP Pancreatitis Rates
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Saadia Nabi, MD
Aventura Hospital
Aventura, FL
Presenting Author(s)
Saadia Nabi, MD1, Aya Akhras, MD1, Kristen Santana, MD1, Luis G. Santiago Zayas, MD1, Ambar Sekulits, MD2, Waseem Wahood, MD3, Sinay Ceballos, MD1, Mohammed Akram, MD1, Henry Manigat, MD3, Daniel Campbell, DO3, Alisha Menon, MD1, Oscar Hernandez, MD3, Franklin Kasmin, MD4
1Aventura Hospital, Aventura, FL; 2Aventura Hospital, Dania Beach, FL; 3HCA Florida Healthcare, Aventura, FL; 4HCA Florida Aventura Hospital and Medical Center, Aventura, FL
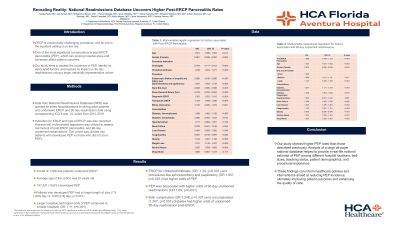
Introduction: ERCP is a technically challenging procedure, and its use in the inpatient setting is on the rise. One of the most significant complications is post-ERCP pancreatitis (PEP), which can prolong hospital stays and adversely affect patient outcomes. Our study aims to assess the incidence of PEP, identify its associated factors, and explore its impact on 90-day readmissions using a large, nationally representative cohort.
Methods: Data from National Readmissions Database (NRD) was queried for index hospitalizations involving adult patients who underwent ERCP and 90-day readmission data using corresponding ICD-9 and -10 codes from 2010-2019. Indication for ERCP and type of ERCP was also recorded. Hierarchical, multivariable regression was utilized to assess risk factors of post-ERCP pancreatitis, and 90-day unplanned readmissions. The cohort was divided into patients who developed PEP vs those who did not (non-PEP).
Results: A total of 1,006,442 patients underwent ERCP. Of these, 167,521 (16.6%) developed PEP. Average age of the cohort was 61 years old. Patients who developed PEP had a longer length of stay (7.9 [±9.8] day vs. 6.08 [±14] day; p< 0.001). Larger hospitals had higher odds of PEP compared to smaller hospitals (OR: 1.11; p< 0.001). ERCP for choledocholithiasis (OR: 1.24; p< 0.001) and procedures like sphincterotomy and papillotomy (OR 1.657, p< 0.001) had higher odds of PEP. PEP was associated with higher odds of 90-day unplanned readmissions (OR 1.09; p< 0.001). Both complicated (OR 1.248, p< 0.001) and uncomplicated (1.207, p< 0.001) diabetes had higher odds of unplanned 90-day readmission post-ERCP.
Discussion: Our study showed higher PEP rates than those described previously. Analysis of a large all-payer national database helped to provide a real-life national estimate of PEP among different hospital locations, bed-sizes, teaching status, patient demographics, and procedural experience. These findings can inform healthcare policies and interventions aimed at reducing PEP incidence, ultimately improving patient outcomes and enhancing the quality of care.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Saadia Nabi, MD1, Aya Akhras, MD1, Kristen Santana, MD1, Luis G. Santiago Zayas, MD1, Ambar Sekulits, MD2, Waseem Wahood, MD3, Sinay Ceballos, MD1, Mohammed Akram, MD1, Henry Manigat, MD3, Daniel Campbell, DO3, Alisha Menon, MD1, Oscar Hernandez, MD3, Franklin Kasmin, MD4. P0035 - Revealing Reality: National Readmissions Database Uncovers Higher Post-ERCP Pancreatitis Rates, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Aventura Hospital, Aventura, FL; 2Aventura Hospital, Dania Beach, FL; 3HCA Florida Healthcare, Aventura, FL; 4HCA Florida Aventura Hospital and Medical Center, Aventura, FL
Introduction: ERCP is a technically challenging procedure, and its use in the inpatient setting is on the rise. One of the most significant complications is post-ERCP pancreatitis (PEP), which can prolong hospital stays and adversely affect patient outcomes. Our study aims to assess the incidence of PEP, identify its associated factors, and explore its impact on 90-day readmissions using a large, nationally representative cohort.
Methods: Data from National Readmissions Database (NRD) was queried for index hospitalizations involving adult patients who underwent ERCP and 90-day readmission data using corresponding ICD-9 and -10 codes from 2010-2019. Indication for ERCP and type of ERCP was also recorded. Hierarchical, multivariable regression was utilized to assess risk factors of post-ERCP pancreatitis, and 90-day unplanned readmissions. The cohort was divided into patients who developed PEP vs those who did not (non-PEP).
Results: A total of 1,006,442 patients underwent ERCP. Of these, 167,521 (16.6%) developed PEP. Average age of the cohort was 61 years old. Patients who developed PEP had a longer length of stay (7.9 [±9.8] day vs. 6.08 [±14] day; p< 0.001). Larger hospitals had higher odds of PEP compared to smaller hospitals (OR: 1.11; p< 0.001). ERCP for choledocholithiasis (OR: 1.24; p< 0.001) and procedures like sphincterotomy and papillotomy (OR 1.657, p< 0.001) had higher odds of PEP. PEP was associated with higher odds of 90-day unplanned readmissions (OR 1.09; p< 0.001). Both complicated (OR 1.248, p< 0.001) and uncomplicated (1.207, p< 0.001) diabetes had higher odds of unplanned 90-day readmission post-ERCP.
Discussion: Our study showed higher PEP rates than those described previously. Analysis of a large all-payer national database helped to provide a real-life national estimate of PEP among different hospital locations, bed-sizes, teaching status, patient demographics, and procedural experience. These findings can inform healthcare policies and interventions aimed at reducing PEP incidence, ultimately improving patient outcomes and enhancing the quality of care.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Saadia Nabi indicated no relevant financial relationships.
Aya Akhras indicated no relevant financial relationships.
Kristen Santana indicated no relevant financial relationships.
Luis Santiago Zayas indicated no relevant financial relationships.
Ambar Sekulits indicated no relevant financial relationships.
Waseem Wahood indicated no relevant financial relationships.
Sinay Ceballos indicated no relevant financial relationships.
Mohammed Akram indicated no relevant financial relationships.
Henry Manigat indicated no relevant financial relationships.
Daniel Campbell indicated no relevant financial relationships.
Alisha Menon indicated no relevant financial relationships.
Oscar Hernandez indicated no relevant financial relationships.
Franklin Kasmin indicated no relevant financial relationships.
Saadia Nabi, MD1, Aya Akhras, MD1, Kristen Santana, MD1, Luis G. Santiago Zayas, MD1, Ambar Sekulits, MD2, Waseem Wahood, MD3, Sinay Ceballos, MD1, Mohammed Akram, MD1, Henry Manigat, MD3, Daniel Campbell, DO3, Alisha Menon, MD1, Oscar Hernandez, MD3, Franklin Kasmin, MD4. P0035 - Revealing Reality: National Readmissions Database Uncovers Higher Post-ERCP Pancreatitis Rates, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
