Sunday Poster Session
Category: Biliary/Pancreas
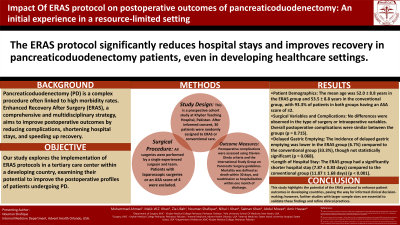
P0038 - Impact of ERAS Protocol on Post-Operative Outcomes of Pancreaticoduodenectomy: An Initial Experience in a Resource-Limited Setting
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Malik W.Z Khan, MD
Yale University School of Medicine
New York, NY
Presenting Author(s)
Muhammad Ahmad, MBBS1, Malik Khan, MD2, Zia Ullah, MBBS3, Nouman Shafique, MD4, Nihal I. Khan, MD4, Salman Khan, MD5, Abdul Moeez, MBBS6, Amir hassan, MBBS7
1Khyber Medical College, Peshawar, North-West Frontier, Pakistan; 2Yale University School of Medicine, New York, NY; 3Khyber Teaching Hospital, Peshawar, North-West Frontier, Pakistan; 4AdventHealth Medical Group, AdventHealth, Orlando, FL; 5Staten Island University Hospital, Northwell Health, New York, NY; 6Khyber Medical College, Mardan, North-West Frontier, Pakistan; 7Bronglais Hospital, Aberystwyth, England, United Kingdom
Introduction: Pancreaticoduodenectomy (PD) is associated with significant morbidity. Enhanced Recovery after Surgery (ERAS) is a multi-faceted and multidisciplinary approach towards improving postoperative outcomes and has been shown to reduce hospital stay and morbidity and accelerate recovery. Our study focuses on the applicability of ERAS in a tertiary care center in a developing country and its impact on the outcome profiles of patients undergoing pancreaticoduodenectomy.
Methods: This is a prospective cohort study at Khyber Teaching Hospital, Pakistan. Initially, 30 patients were included in the study; after informed consent, they were randomly assigned to the ERAS and conventional cohorts. Patients undergoing pancreatic surgery were included, with the exception of those who had laparoscopic surgeries or had an American Society of Anesthesiology score of 4. All surgical procedures were performed by a single experienced surgeon and his team. Postoperative complications were defined according to Clavien-Dindo criteria and the International Study Group on Pancreatic Surgery. Mortality was defined as any death occurring within 30 days of surgery, and readmission was defined as admission to the hospital within one month of discharge.
Results: The mean age of patients in the ERAS group was 52.0 ± 8.8 years, while that of the conventional group was 53.5 ± 8.8 years. The majority of patients (93.3%) in both groups had an ASA score of ≤2. There were no differences in the type of surgery or intraoperative variables. Postoperative complications were similar in both groups (p = 0.715); however, the incidence of delayed gastric emptying was lower in the ERAS group 1 (6.7%) compared to the conventional group 5 (33.3%), though statistically insignificant (p = 0.068). The length of hospital stay (LOS) was 7.87 ± 0.83 days in the ERAS group and 11.87 ± 1.68 days in the conventional group (p< 0.001).
Discussion: This study demonstrates that the ERAS protocol can be safely and effectively implemented in a developing country as it improves patient outcomes and produces a substantial decrease in the length of hospital stay. Further studies with larger sample sizes are required to validate these findings and guide clinical decision-making.
Disclosures:
Muhammad Ahmad, MBBS1, Malik Khan, MD2, Zia Ullah, MBBS3, Nouman Shafique, MD4, Nihal I. Khan, MD4, Salman Khan, MD5, Abdul Moeez, MBBS6, Amir hassan, MBBS7. P0038 - Impact of ERAS Protocol on Post-Operative Outcomes of Pancreaticoduodenectomy: An Initial Experience in a Resource-Limited Setting, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Khyber Medical College, Peshawar, North-West Frontier, Pakistan; 2Yale University School of Medicine, New York, NY; 3Khyber Teaching Hospital, Peshawar, North-West Frontier, Pakistan; 4AdventHealth Medical Group, AdventHealth, Orlando, FL; 5Staten Island University Hospital, Northwell Health, New York, NY; 6Khyber Medical College, Mardan, North-West Frontier, Pakistan; 7Bronglais Hospital, Aberystwyth, England, United Kingdom
Introduction: Pancreaticoduodenectomy (PD) is associated with significant morbidity. Enhanced Recovery after Surgery (ERAS) is a multi-faceted and multidisciplinary approach towards improving postoperative outcomes and has been shown to reduce hospital stay and morbidity and accelerate recovery. Our study focuses on the applicability of ERAS in a tertiary care center in a developing country and its impact on the outcome profiles of patients undergoing pancreaticoduodenectomy.
Methods: This is a prospective cohort study at Khyber Teaching Hospital, Pakistan. Initially, 30 patients were included in the study; after informed consent, they were randomly assigned to the ERAS and conventional cohorts. Patients undergoing pancreatic surgery were included, with the exception of those who had laparoscopic surgeries or had an American Society of Anesthesiology score of 4. All surgical procedures were performed by a single experienced surgeon and his team. Postoperative complications were defined according to Clavien-Dindo criteria and the International Study Group on Pancreatic Surgery. Mortality was defined as any death occurring within 30 days of surgery, and readmission was defined as admission to the hospital within one month of discharge.
Results: The mean age of patients in the ERAS group was 52.0 ± 8.8 years, while that of the conventional group was 53.5 ± 8.8 years. The majority of patients (93.3%) in both groups had an ASA score of ≤2. There were no differences in the type of surgery or intraoperative variables. Postoperative complications were similar in both groups (p = 0.715); however, the incidence of delayed gastric emptying was lower in the ERAS group 1 (6.7%) compared to the conventional group 5 (33.3%), though statistically insignificant (p = 0.068). The length of hospital stay (LOS) was 7.87 ± 0.83 days in the ERAS group and 11.87 ± 1.68 days in the conventional group (p< 0.001).
Discussion: This study demonstrates that the ERAS protocol can be safely and effectively implemented in a developing country as it improves patient outcomes and produces a substantial decrease in the length of hospital stay. Further studies with larger sample sizes are required to validate these findings and guide clinical decision-making.
Disclosures:
Muhammad Ahmad indicated no relevant financial relationships.
Malik Khan indicated no relevant financial relationships.
Zia Ullah indicated no relevant financial relationships.
Nouman Shafique indicated no relevant financial relationships.
Nihal Khan indicated no relevant financial relationships.
Salman Khan indicated no relevant financial relationships.
Abdul Moeez indicated no relevant financial relationships.
Amir hassan indicated no relevant financial relationships.
Muhammad Ahmad, MBBS1, Malik Khan, MD2, Zia Ullah, MBBS3, Nouman Shafique, MD4, Nihal I. Khan, MD4, Salman Khan, MD5, Abdul Moeez, MBBS6, Amir hassan, MBBS7. P0038 - Impact of ERAS Protocol on Post-Operative Outcomes of Pancreaticoduodenectomy: An Initial Experience in a Resource-Limited Setting, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
