Sunday Poster Session
Category: Biliary/Pancreas
P0041 - Pain Medication Use in Chronic Pancreatitis Patients Undergoing ERCP
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Carolyn Brooks, MD
Emory University School of Medicine
Atlanta, GA
Presenting Author(s)
Carolyn Brooks, MD1, Rishi Das, MD, MPH1, Ikenna K.. Emelogu, MD1, Wenyi Wang, BS2, Steven Keilin, MD1, Vaishali Patel, MD, MHS1, Field Willingham, MD, MPH1, Jordan Orr, MD1, Saurabh Chawla, MD1
1Emory University School of Medicine, Atlanta, GA; 2Emory Rollins School of Public Health, Atlanta, GA
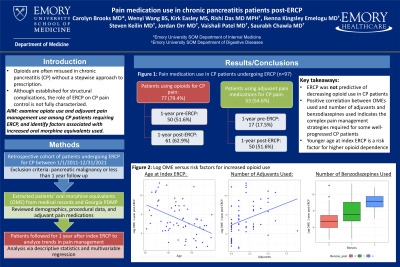
Introduction: Opioids are often prescribed for abdominal pain in chronic pancreatitis (CP), which can lead to dependence and misuse. ERCP for management of structural disease complications may help with pain control, but it is poorly understood which factors contribute to uncontrolled pain before and after the procedure. The aim of our study was to investigate opiate and adjuvant pain medication use among CP patients requiring ERCP and identify risk factors for increased pain control needs.
Methods: We performed a retrospective cohort study of CP patients undergoing ERCP between 1/1/2011 to 12/31/2021, excluding patients with pancreatic malignancy or less than 1 year follow-up. Patients’ opioid prescriptions of 30+ days were obtained from medical records and the Georgia Prescription Drug Monitoring Program, and oral morphine equivalents (OME) used in the 1 year before and after patients’ first ERCP were calculated. Demographics, ERCP data, and adjuvant pain medications (gabapentinoids, TCAs, anticholinergics, antispasmodics) were reviewed. Descriptive statistics and univariate linear regression were used for assessment.
Results: Of the 97 patients who met the inclusion criteria, 79.38% used opioids chronically for CP pain. The number of patients using opioids increased from 1 year before index ERCP (51.55%) to 1 year after (62.89%). The number of patients using adjuvant pain medications also increased in the year after index ERCP (17.53% to 51.55%).
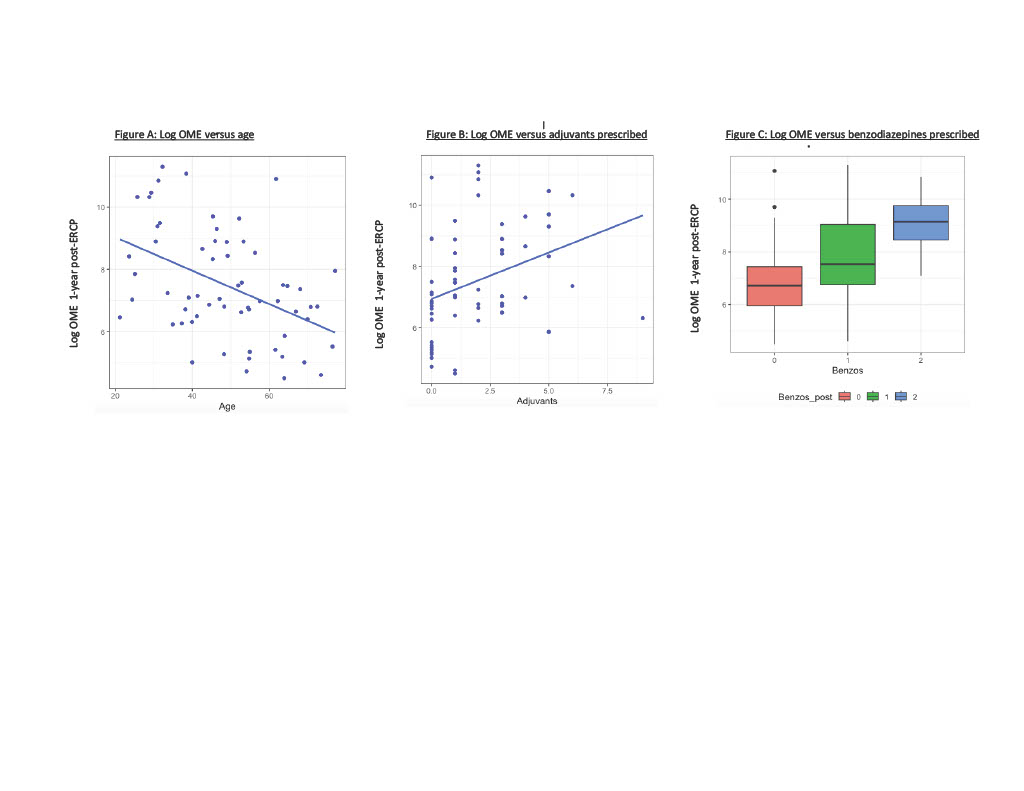
Younger age at index ERCP was associated with an increase in total OMEs used 1 year post-index ERCP (β=-0.05, [CI -0.08, -0.03]). Increased benzodiazepine use and increased adjuvant pain medication use were also correlated with increased OMEs 1 year after index ERCP (β=1.02 [0.33, 1.70], β=0.30 [0.09, 0.51] respectively). Smoking history was associated with an increase in OMEs used in the 1-year post-index ERCP, but the association was not significant. Race, gender, and the various etiologies for chronic pancreatitis or indication for ERCP did not impact OME consumption.
Discussion: ERCP did not result in a decrease in opioid use in CP patients. Increasing opiate use and adjuvant pain medication use 1-year post-ERCP, and the positive correlation between OMEs and number of adjuvants and benzodiazepines used, indicates there is a population of CP patients with a complex pain management picture requiring multi-disciplinary coordination. Younger age at index ERCP may also be a risk factor for higher opiate dependence in CP.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Carolyn Brooks, MD1, Rishi Das, MD, MPH1, Ikenna K.. Emelogu, MD1, Wenyi Wang, BS2, Steven Keilin, MD1, Vaishali Patel, MD, MHS1, Field Willingham, MD, MPH1, Jordan Orr, MD1, Saurabh Chawla, MD1. P0041 - Pain Medication Use in Chronic Pancreatitis Patients Undergoing ERCP, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Emory University School of Medicine, Atlanta, GA; 2Emory Rollins School of Public Health, Atlanta, GA
Introduction: Opioids are often prescribed for abdominal pain in chronic pancreatitis (CP), which can lead to dependence and misuse. ERCP for management of structural disease complications may help with pain control, but it is poorly understood which factors contribute to uncontrolled pain before and after the procedure. The aim of our study was to investigate opiate and adjuvant pain medication use among CP patients requiring ERCP and identify risk factors for increased pain control needs.
Methods: We performed a retrospective cohort study of CP patients undergoing ERCP between 1/1/2011 to 12/31/2021, excluding patients with pancreatic malignancy or less than 1 year follow-up. Patients’ opioid prescriptions of 30+ days were obtained from medical records and the Georgia Prescription Drug Monitoring Program, and oral morphine equivalents (OME) used in the 1 year before and after patients’ first ERCP were calculated. Demographics, ERCP data, and adjuvant pain medications (gabapentinoids, TCAs, anticholinergics, antispasmodics) were reviewed. Descriptive statistics and univariate linear regression were used for assessment.
Results: Of the 97 patients who met the inclusion criteria, 79.38% used opioids chronically for CP pain. The number of patients using opioids increased from 1 year before index ERCP (51.55%) to 1 year after (62.89%). The number of patients using adjuvant pain medications also increased in the year after index ERCP (17.53% to 51.55%).
Younger age at index ERCP was associated with an increase in total OMEs used 1 year post-index ERCP (β=-0.05, [CI -0.08, -0.03]). Increased benzodiazepine use and increased adjuvant pain medication use were also correlated with increased OMEs 1 year after index ERCP (β=1.02 [0.33, 1.70], β=0.30 [0.09, 0.51] respectively). Smoking history was associated with an increase in OMEs used in the 1-year post-index ERCP, but the association was not significant. Race, gender, and the various etiologies for chronic pancreatitis or indication for ERCP did not impact OME consumption.
Discussion: ERCP did not result in a decrease in opioid use in CP patients. Increasing opiate use and adjuvant pain medication use 1-year post-ERCP, and the positive correlation between OMEs and number of adjuvants and benzodiazepines used, indicates there is a population of CP patients with a complex pain management picture requiring multi-disciplinary coordination. Younger age at index ERCP may also be a risk factor for higher opiate dependence in CP.
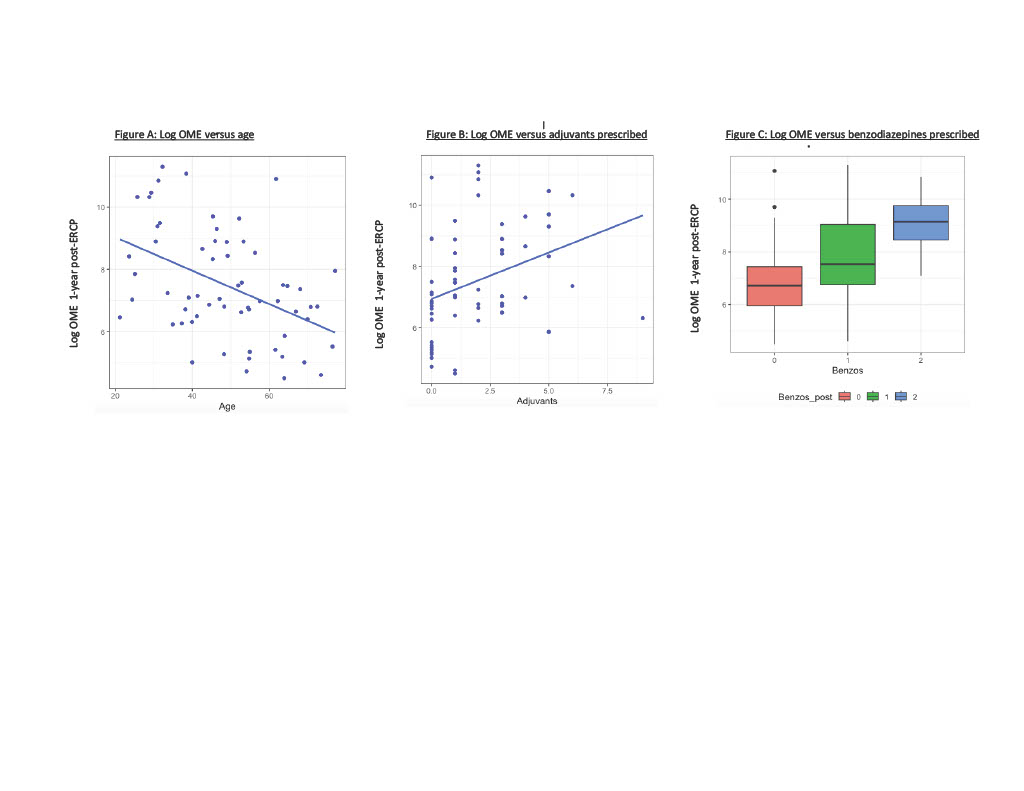
Figure: Factors influencing OMEs used 1-year post ERCP
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Carolyn Brooks indicated no relevant financial relationships.
Rishi Das indicated no relevant financial relationships.
Ikenna Emelogu indicated no relevant financial relationships.
Wenyi Wang indicated no relevant financial relationships.
Steven Keilin indicated no relevant financial relationships.
Vaishali Patel indicated no relevant financial relationships.
Field Willingham indicated no relevant financial relationships.
Jordan Orr indicated no relevant financial relationships.
Saurabh Chawla indicated no relevant financial relationships.
Carolyn Brooks, MD1, Rishi Das, MD, MPH1, Ikenna K.. Emelogu, MD1, Wenyi Wang, BS2, Steven Keilin, MD1, Vaishali Patel, MD, MHS1, Field Willingham, MD, MPH1, Jordan Orr, MD1, Saurabh Chawla, MD1. P0041 - Pain Medication Use in Chronic Pancreatitis Patients Undergoing ERCP, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
