Sunday Poster Session
Category: Biliary/Pancreas
P0043 - COVID-19 Vaccine-Induced Acute Pancreatitis: A Systematic Review
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
- AG
Amlish Gondal, MD
Guthrie Robert Packer Hospital
Sayre, PA
Presenting Author(s)
Mahrukh Tariq, MBBS1, Amlish Gondal, MD2, Gaurang H.. Suhagiya, MBBS3, Priyank M. Dholakiya, MBBS4, Fnu Girish, MBBS5, Aman Kumar, MBBS5, Diksha Suchwani, MBBS5, Kajal Bai, MBBS6, Tazeen Nazar, MBBS7, Bilal Aziz, MBBS7, Zahoor Ahmed, MD8
1Rawalpindi Medical University, Rawalpindi, Punjab, Pakistan; 2Guthrie Robert Packer Hospital, Sayre, PA; 3Jiangsu University, Zhenjiang, Jiangsu, China; 4GMERS Medical College and Hospital, Amreli, Gujarat, India; 5Ghulam Muhammad Mahar Medical College, Sukkur, Sindh, Pakistan; 6Chandka Medical College, Larkana, Sindh, Pakistan; 7King Edward Medical University, Lahore, Punjab, Pakistan; 8Rochester General Hospital, Rochester, NY
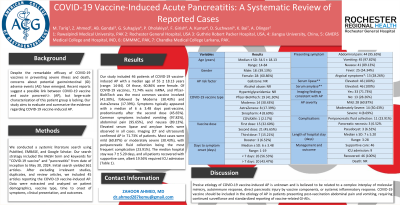
Introduction: Despite the remarkable efficacy of COVID-19 vaccines in preventing severe illness and death, concerns about potential gastrointestinal (GI) adverse events (AE) have emerged. Recent reports suggest a possible link between COVID-19 vaccine and acute pancreatitis (AP), but large-scale characterization of this patient group is lacking. Our study aims to evaluate and summarize the evidence regarding COVID-19 vaccine-induced AP.
Methods: We conducted a systemic literature search using PubMed, EMBASE, and Google Scholar. Our search strategy included the MeSH term and keywords for "COVID-19 vaccine" and "pancreatitis" from date of inception to May 30, 2024. Initial search yielded 361 articles. After excluding irrelevant studies, duplicates, and review articles, we included 45 articles reporting the COVID-19 vaccine-induced AP. Data were extracted and analyzed on patient demographics, vaccine type, time to onset of symptoms, clinical presentation, and outcomes.
Results: Our study included 46 patients of COVID-19 vaccine-induced AP with a median age of 55 ± 18.13 years (range: 14-84). Of those, 60.86% were female. Of COVID-19 vaccines, 71.74% were mRNA, and Pfizer-BioNTech was the most common vaccine involved (41.30%), followed by Moderna (30.43%) and AstraZeneca (17.39%). Symptoms typically appeared with a median of 6 ± 3.48 days post-vaccine, predominantly after the second dose (45.65%). Common symptoms included vomiting (97.82%), abdominal pain (95.65%), and nausea (89.13%). Elevated serum lipase and amylase levels were observed in all cases. Imaging (CT and ultrasound) confirmed AP in 71.73% of patients. Most cases were mild (60.87%) or moderately severe (30.43%), with peripancreatic fluid collection being the most frequent complication (23.91%). The median hospital stay was 7 ± 5.20 days, and all patients recovered with supportive care, albeit 19.56% required ICU admission (Table 1).
Discussion: Precise etiology of COVID-19 vaccine-induced AP is unknown and is believed to be related to a complex interplay of molecular mimicry, autoimmune response, direct pancreatic injury by vaccine components, or systemic inflammatory response. Albeit rare, AP is a life-threatening complication of the COVID-19 vaccine, warranting urgent evaluation and management. COVID-19 vaccine should be included in the etiology of AP in patients presenting post-vaccination abdominal pain and vomiting, requiring continued surveillance and standardized reporting of vaccine-related GI-AEs.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mahrukh Tariq, MBBS1, Amlish Gondal, MD2, Gaurang H.. Suhagiya, MBBS3, Priyank M. Dholakiya, MBBS4, Fnu Girish, MBBS5, Aman Kumar, MBBS5, Diksha Suchwani, MBBS5, Kajal Bai, MBBS6, Tazeen Nazar, MBBS7, Bilal Aziz, MBBS7, Zahoor Ahmed, MD8. P0043 - COVID-19 Vaccine-Induced Acute Pancreatitis: A Systematic Review, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Rawalpindi Medical University, Rawalpindi, Punjab, Pakistan; 2Guthrie Robert Packer Hospital, Sayre, PA; 3Jiangsu University, Zhenjiang, Jiangsu, China; 4GMERS Medical College and Hospital, Amreli, Gujarat, India; 5Ghulam Muhammad Mahar Medical College, Sukkur, Sindh, Pakistan; 6Chandka Medical College, Larkana, Sindh, Pakistan; 7King Edward Medical University, Lahore, Punjab, Pakistan; 8Rochester General Hospital, Rochester, NY
Introduction: Despite the remarkable efficacy of COVID-19 vaccines in preventing severe illness and death, concerns about potential gastrointestinal (GI) adverse events (AE) have emerged. Recent reports suggest a possible link between COVID-19 vaccine and acute pancreatitis (AP), but large-scale characterization of this patient group is lacking. Our study aims to evaluate and summarize the evidence regarding COVID-19 vaccine-induced AP.
Methods: We conducted a systemic literature search using PubMed, EMBASE, and Google Scholar. Our search strategy included the MeSH term and keywords for "COVID-19 vaccine" and "pancreatitis" from date of inception to May 30, 2024. Initial search yielded 361 articles. After excluding irrelevant studies, duplicates, and review articles, we included 45 articles reporting the COVID-19 vaccine-induced AP. Data were extracted and analyzed on patient demographics, vaccine type, time to onset of symptoms, clinical presentation, and outcomes.
Results: Our study included 46 patients of COVID-19 vaccine-induced AP with a median age of 55 ± 18.13 years (range: 14-84). Of those, 60.86% were female. Of COVID-19 vaccines, 71.74% were mRNA, and Pfizer-BioNTech was the most common vaccine involved (41.30%), followed by Moderna (30.43%) and AstraZeneca (17.39%). Symptoms typically appeared with a median of 6 ± 3.48 days post-vaccine, predominantly after the second dose (45.65%). Common symptoms included vomiting (97.82%), abdominal pain (95.65%), and nausea (89.13%). Elevated serum lipase and amylase levels were observed in all cases. Imaging (CT and ultrasound) confirmed AP in 71.73% of patients. Most cases were mild (60.87%) or moderately severe (30.43%), with peripancreatic fluid collection being the most frequent complication (23.91%). The median hospital stay was 7 ± 5.20 days, and all patients recovered with supportive care, albeit 19.56% required ICU admission (Table 1).
Discussion: Precise etiology of COVID-19 vaccine-induced AP is unknown and is believed to be related to a complex interplay of molecular mimicry, autoimmune response, direct pancreatic injury by vaccine components, or systemic inflammatory response. Albeit rare, AP is a life-threatening complication of the COVID-19 vaccine, warranting urgent evaluation and management. COVID-19 vaccine should be included in the etiology of AP in patients presenting post-vaccination abdominal pain and vomiting, requiring continued surveillance and standardized reporting of vaccine-related GI-AEs.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mahrukh Tariq indicated no relevant financial relationships.
Amlish Gondal indicated no relevant financial relationships.
Gaurang Suhagiya indicated no relevant financial relationships.
Priyank Dholakiya indicated no relevant financial relationships.
Fnu Girish indicated no relevant financial relationships.
Aman Kumar indicated no relevant financial relationships.
Diksha Suchwani indicated no relevant financial relationships.
Kajal Bai indicated no relevant financial relationships.
Tazeen Nazar indicated no relevant financial relationships.
Bilal Aziz indicated no relevant financial relationships.
Zahoor Ahmed indicated no relevant financial relationships.
Mahrukh Tariq, MBBS1, Amlish Gondal, MD2, Gaurang H.. Suhagiya, MBBS3, Priyank M. Dholakiya, MBBS4, Fnu Girish, MBBS5, Aman Kumar, MBBS5, Diksha Suchwani, MBBS5, Kajal Bai, MBBS6, Tazeen Nazar, MBBS7, Bilal Aziz, MBBS7, Zahoor Ahmed, MD8. P0043 - COVID-19 Vaccine-Induced Acute Pancreatitis: A Systematic Review, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
