Sunday Poster Session
Category: Biliary/Pancreas
P0065 - Diagnostic Value of Anti-Mitochondrial Antibodies (AMA), Anti-M2, Anti-sp100, and Anti-gp210 in Primary Biliary Cholangitis (PBC)
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- JY
Jane Yang, MD
Labcorp
Calabasas, CA
Presenting Author(s)
Jane Yang, MD1, Ato O Aikins, PhD2, Rubio Punzalan, MD, PhD1, David Alfego, PhD2, Kelly Chun, PhD1
1Labcorp, Calabasas, CA; 2Labcorp, Burlington, NC
Introduction: Anti-mitochondrial antibodies (AMA) are the serologic hallmark of Primary Biliary Cholangitis (PBC), a chronic liver disease characterized by immune-mediated destruction of intrahepatic bile ducts.1 Most presenting patients are asymptomatic. If undiagnosed and untreated, a substantial number progress to liver fibrosis and liver failure within 10 years. In the setting of an otherwise unexplained persistent alkaline phosphatase elevation, the diagnosis of PBC can be established with 1) liver histology consistent with PBC or 2) the presence of AMA or other PBC-specific autoantibodies such as anti-sp100 or anti-gp210.1 Here, we present results of a comprehensive diagnostic PBC profile comprised of AMA and anti-nuclear antibodies (ANA) by indirect immunofluorescence assay (IFA) and anti-mitochondrial M2, anti-sp100 and anti-gp210 in 1933 patient serum samples.
Methods: Enzyme immunosorbent assays (ELISAs) utilize nuclear body sp100, nuclear pore membrane gp210, and recombinant M2 called MIT3 which incorporates the 3 immunodominant epitopes of the E2 subunit of the pyruvate dehydrogenase complex found in mitochondria. ANA and AMA by IFA utilize human epithelial cells, HEp2, and mouse kidney/stomach/liver tissue, respectively, and fluorescein-labeled anti-human IgG conjugate; patterns are visualized through a fluorescence microscope.
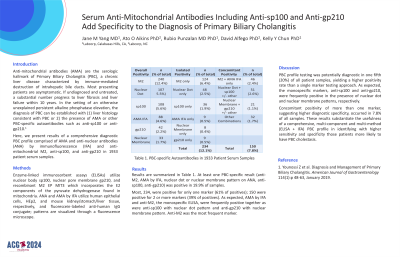
Results: Results are summarized in Table 1. At least one PBC-specific result (anti-M2, AMA by IFA, nuclear dot or nuclear membrane pattern on ANA, anti-sp100, anti-gp210) was positive in 19.9% of samples. Most, 234, were positive for only one marker; 150 were positive for 2 or more markers. As expected, AMA by IFA and anti-M2, the monospecific ELISA, were frequently positive together as were anti-sp100 with nuclear dot pattern and anti-gp210 with nuclear membrane pattern. Anti-M2 was the most frequent marker.
Discussion: PBC profile testing was potentially diagnostic in one fifth (20%) of all patient samples, yielding a higher positivity rate than a single marker testing approach. Concomitant positivity of more than one marker, suggesting higher diagnostic specificity, occurred in 7.8%. These results substantiate the usefulness of a comprehensive, multi-component and multi-method (ELISA + IFA) PBC profile in identifying with higher sensitivity and specificity those patients more likely to have PBC cholestasis.
1. Younossi Z et al. Diagnosis and Management of Primary Biliary Cholangitis. Am J Gastroenterol 114(1):p 48-63, January 2019.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jane Yang, MD1, Ato O Aikins, PhD2, Rubio Punzalan, MD, PhD1, David Alfego, PhD2, Kelly Chun, PhD1. P0065 - Diagnostic Value of Anti-Mitochondrial Antibodies (AMA), Anti-M2, Anti-sp100, and Anti-gp210 in Primary Biliary Cholangitis (PBC), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Labcorp, Calabasas, CA; 2Labcorp, Burlington, NC
Introduction: Anti-mitochondrial antibodies (AMA) are the serologic hallmark of Primary Biliary Cholangitis (PBC), a chronic liver disease characterized by immune-mediated destruction of intrahepatic bile ducts.1 Most presenting patients are asymptomatic. If undiagnosed and untreated, a substantial number progress to liver fibrosis and liver failure within 10 years. In the setting of an otherwise unexplained persistent alkaline phosphatase elevation, the diagnosis of PBC can be established with 1) liver histology consistent with PBC or 2) the presence of AMA or other PBC-specific autoantibodies such as anti-sp100 or anti-gp210.1 Here, we present results of a comprehensive diagnostic PBC profile comprised of AMA and anti-nuclear antibodies (ANA) by indirect immunofluorescence assay (IFA) and anti-mitochondrial M2, anti-sp100 and anti-gp210 in 1933 patient serum samples.
Methods: Enzyme immunosorbent assays (ELISAs) utilize nuclear body sp100, nuclear pore membrane gp210, and recombinant M2 called MIT3 which incorporates the 3 immunodominant epitopes of the E2 subunit of the pyruvate dehydrogenase complex found in mitochondria. ANA and AMA by IFA utilize human epithelial cells, HEp2, and mouse kidney/stomach/liver tissue, respectively, and fluorescein-labeled anti-human IgG conjugate; patterns are visualized through a fluorescence microscope.
Results: Results are summarized in Table 1. At least one PBC-specific result (anti-M2, AMA by IFA, nuclear dot or nuclear membrane pattern on ANA, anti-sp100, anti-gp210) was positive in 19.9% of samples. Most, 234, were positive for only one marker; 150 were positive for 2 or more markers. As expected, AMA by IFA and anti-M2, the monospecific ELISA, were frequently positive together as were anti-sp100 with nuclear dot pattern and anti-gp210 with nuclear membrane pattern. Anti-M2 was the most frequent marker.
Discussion: PBC profile testing was potentially diagnostic in one fifth (20%) of all patient samples, yielding a higher positivity rate than a single marker testing approach. Concomitant positivity of more than one marker, suggesting higher diagnostic specificity, occurred in 7.8%. These results substantiate the usefulness of a comprehensive, multi-component and multi-method (ELISA + IFA) PBC profile in identifying with higher sensitivity and specificity those patients more likely to have PBC cholestasis.
1. Younossi Z et al. Diagnosis and Management of Primary Biliary Cholangitis. Am J Gastroenterol 114(1):p 48-63, January 2019.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jane Yang indicated no relevant financial relationships.
Ato O Aikins indicated no relevant financial relationships.
Rubio Punzalan indicated no relevant financial relationships.
David Alfego indicated no relevant financial relationships.
Kelly Chun indicated no relevant financial relationships.
Jane Yang, MD1, Ato O Aikins, PhD2, Rubio Punzalan, MD, PhD1, David Alfego, PhD2, Kelly Chun, PhD1. P0065 - Diagnostic Value of Anti-Mitochondrial Antibodies (AMA), Anti-M2, Anti-sp100, and Anti-gp210 in Primary Biliary Cholangitis (PBC), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
