Sunday Poster Session
Category: Biliary/Pancreas
P0066 - Anticoagulation in Acute Pancreatitis Related Thrombosis: Practice Variations
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Naomi Reddy-Patel, MD
St. Luke's University Hospital
Bethlehem, PA
Presenting Author(s)
Naomi Reddy-Patel, MD1, Janak Bahirwani, MD2, Frank Lin, DO3, Emilie Kim, MD1, Kimberly Chaput, DO2
1St. Luke's University Hospital, Bethlehem, PA; 2St. Luke's University Health Network, Bethlehem, PA; 3St. Luke's University Health Network, Allentown, PA
Introduction: Pancreatitis-induced thrombosis is a notable complication of pancreatic inflammation, where the inflammation can extend to the splenic, portal, or superior mesenteric veins (SMV) leading to thrombus formation. The acute inflammation resolves with appropriate treatment of the underlying pancreatic condition, suggesting that complications associated with vein inflammation can also be mitigated without initiation of anticoagulation. This study aims to investigate whether patients admitted with acute pancreatitis and diagnosed with a thrombus are initiated on anticoagulation therapy and the complications associated with that
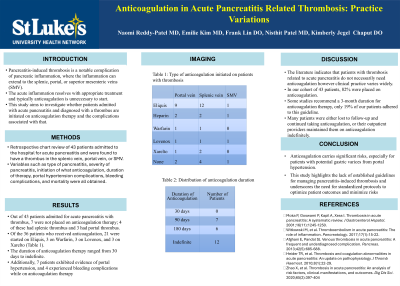
Methods: This is a retrospective chart review on 43 patients admitted to the hospital for acute pancreatitis and were found to have a thrombus in the splenic vein, portal vein, or SMV. Variables such as type of pancreatitis, severity of pancreatitis, initiation of what anticoagulation, duration of therapy, portal hypertension complications, bleeding complications, and mortality were all obtained
Results: Out of 43 patients admitted for acute pancreatitis with thrombus, 7 were not placed on anticoagulation therapy; 4 of these had splenic thrombus and 3 had portal thrombus. Of the 36 patients who received anticoagulation, 21 were started on Eliquis, 3 on Warfarin, 3 on Lovenox, and 3 on Xarelto. The duration of anticoagulation therapy ranged from 30 days to indefinite. 12 patients were placed on indefinite anticoagulation, although only 3 had a history necessitating prolonged anticoagulation. 7 patients were placed on anticoagulation for 90 days, and 6 for 180 days. Additionally, 7 patients exhibited evidence of portal hypertension, and 4 experienced bleeding complications while on anticoagulation therapy
Discussion: While the literature indicates that patients with thrombosis related to acute pancreatitis do not need anticoagulation, clinical practice varies widely. of our 43 patients, 82% were placed on anticoagulation. Although some studies recommend a 3-month duration for anticoagulation therapy, only 19% of our patients adhered to this guideline. Many patients were either lost to follow-up and continued taking anticoagulation indefinitely, or their outpatient providers maintained them on anticoagulation indefinitely. Anticoagulation carries significant risks and this study highlights the lack of established guidelines for managing pancreatitis-induced thrombosis and underscores the need for standardized protocols to optimize patient outcomes and minimize risks
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Naomi Reddy-Patel, MD1, Janak Bahirwani, MD2, Frank Lin, DO3, Emilie Kim, MD1, Kimberly Chaput, DO2. P0066 - Anticoagulation in Acute Pancreatitis Related Thrombosis: Practice Variations, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1St. Luke's University Hospital, Bethlehem, PA; 2St. Luke's University Health Network, Bethlehem, PA; 3St. Luke's University Health Network, Allentown, PA
Introduction: Pancreatitis-induced thrombosis is a notable complication of pancreatic inflammation, where the inflammation can extend to the splenic, portal, or superior mesenteric veins (SMV) leading to thrombus formation. The acute inflammation resolves with appropriate treatment of the underlying pancreatic condition, suggesting that complications associated with vein inflammation can also be mitigated without initiation of anticoagulation. This study aims to investigate whether patients admitted with acute pancreatitis and diagnosed with a thrombus are initiated on anticoagulation therapy and the complications associated with that
Methods: This is a retrospective chart review on 43 patients admitted to the hospital for acute pancreatitis and were found to have a thrombus in the splenic vein, portal vein, or SMV. Variables such as type of pancreatitis, severity of pancreatitis, initiation of what anticoagulation, duration of therapy, portal hypertension complications, bleeding complications, and mortality were all obtained
Results: Out of 43 patients admitted for acute pancreatitis with thrombus, 7 were not placed on anticoagulation therapy; 4 of these had splenic thrombus and 3 had portal thrombus. Of the 36 patients who received anticoagulation, 21 were started on Eliquis, 3 on Warfarin, 3 on Lovenox, and 3 on Xarelto. The duration of anticoagulation therapy ranged from 30 days to indefinite. 12 patients were placed on indefinite anticoagulation, although only 3 had a history necessitating prolonged anticoagulation. 7 patients were placed on anticoagulation for 90 days, and 6 for 180 days. Additionally, 7 patients exhibited evidence of portal hypertension, and 4 experienced bleeding complications while on anticoagulation therapy
Discussion: While the literature indicates that patients with thrombosis related to acute pancreatitis do not need anticoagulation, clinical practice varies widely. of our 43 patients, 82% were placed on anticoagulation. Although some studies recommend a 3-month duration for anticoagulation therapy, only 19% of our patients adhered to this guideline. Many patients were either lost to follow-up and continued taking anticoagulation indefinitely, or their outpatient providers maintained them on anticoagulation indefinitely. Anticoagulation carries significant risks and this study highlights the lack of established guidelines for managing pancreatitis-induced thrombosis and underscores the need for standardized protocols to optimize patient outcomes and minimize risks
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Naomi Reddy-Patel indicated no relevant financial relationships.
Janak Bahirwani indicated no relevant financial relationships.
Frank Lin indicated no relevant financial relationships.
Emilie Kim indicated no relevant financial relationships.
Kimberly Chaput indicated no relevant financial relationships.
Naomi Reddy-Patel, MD1, Janak Bahirwani, MD2, Frank Lin, DO3, Emilie Kim, MD1, Kimberly Chaput, DO2. P0066 - Anticoagulation in Acute Pancreatitis Related Thrombosis: Practice Variations, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
