Sunday Poster Session
Category: Biliary/Pancreas
P0070 - Comparative Analysis of ERCP and PTBD for Biliary Interventions for Readmission Rates and Patient Outcomes
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Daniel Wang, MD
Keck School of Medicine of the University of Southern California
Torrance, CA
Presenting Author(s)
Daniel Wang, MD1, Patrick Chang, MD2, Supisara Tintara, MD2, Frederick Chang, DO3, Jennifer Phan, MD2
1Keck School of Medicine of the University of Southern California, Torrance, CA; 2University of Southern California, Los Angeles, CA; 3University of Arizona, Phoenix, AZ
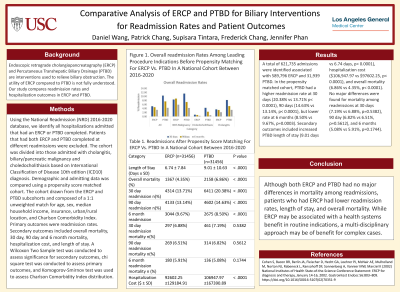
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) and Percutaneous Transhepatic Biliary Drainage (PTBD) are interventions used to relieve biliary obstruction. The utility of ERCP compared to PTBD is not fully understood. Our study compares readmission rates and hospitalization outcomes in ERCP and PTBD.
Methods: Using the National Readmission (NRD) 2016-2020 database, we identify all hospitalizations admitted that had an ERCP or PTBD completed. Patients that had both ERCP and PTBD completed at different readmissions were excluded. The cohort was divided into those admitted with cholangitis, biliary/pancreatic malignancy and choledocholithiasis based on International Classification of Disease 10th edition (ICD10) diagnosis. Demographic and admitting data was compared using a propensity score matched cohort. The cohort drawn from the ERCP and PTBD subcohorts and composed of a 1:1 unweighted match for age, sex, median household income, insurance, urban/rural location, and Charlson Comorbidity Index. Primary outcomes were readmission rates. Secondary outcomes included overall mortality, 30 day, 90 day and 6 month mortality, hospitalization cost, and length of stay. A Wilcoxon Two Sample test was conducted to assess significance for secondary outcomes, chi square test was conducted to assess primary outcomes, and Komogorov-Smirnov test was used to assess Charlson Comorbidity Index distribution.
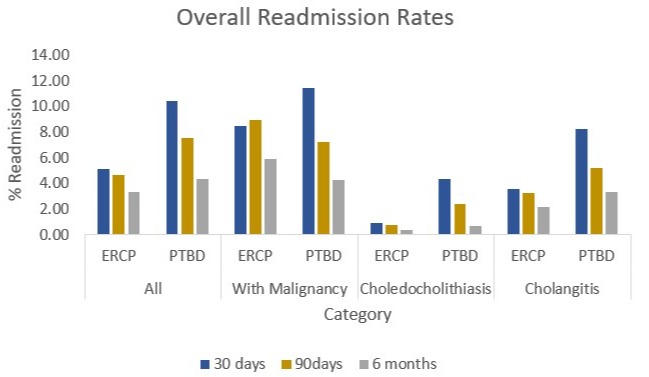
Results: A total of 621,735 admissions were identified associated with 589,796 ERCP and 31,939 PTBD. In the propensity matched cohort, PTBD had a higher readmission rate at 30 days (20.38% vs 13.71% p< 0.0001), 90 days (14.63% vs 13.14%, p< 0.0001), but lower rate at 6 months (8.50% vs 9.67%, p=0.0003). Secondary outcomes included increased PTBD length of stay (9.01 days vs 6.74 days, p< 0.0001), hospitalization cost ($106,947.97 vs $97602.25, p< 0.0001), and overall mortality (6.86% vs 4.35%, p< 0.0001). No major differences were found for mortality among readmissions at 30 days (7.19% vs 6.88%, p=0.5382), 90 day (6.82% vs 6.51%, p=0.5612), and 6 months (5.08% vs 5.91%, p=0.1744).
Discussion: Although both ERCP and PTBD had no major differences in mortality among readmissions, patients who had ERCP had lower readmission rates, length of stay, and overall mortality. While ERCP may be associated with a health systems benefit in routine indications, a multi-disciplinary approach may be of benefit for complex cases.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Daniel Wang, MD1, Patrick Chang, MD2, Supisara Tintara, MD2, Frederick Chang, DO3, Jennifer Phan, MD2. P0070 - Comparative Analysis of ERCP and PTBD for Biliary Interventions for Readmission Rates and Patient Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Keck School of Medicine of the University of Southern California, Torrance, CA; 2University of Southern California, Los Angeles, CA; 3University of Arizona, Phoenix, AZ
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) and Percutaneous Transhepatic Biliary Drainage (PTBD) are interventions used to relieve biliary obstruction. The utility of ERCP compared to PTBD is not fully understood. Our study compares readmission rates and hospitalization outcomes in ERCP and PTBD.
Methods: Using the National Readmission (NRD) 2016-2020 database, we identify all hospitalizations admitted that had an ERCP or PTBD completed. Patients that had both ERCP and PTBD completed at different readmissions were excluded. The cohort was divided into those admitted with cholangitis, biliary/pancreatic malignancy and choledocholithiasis based on International Classification of Disease 10th edition (ICD10) diagnosis. Demographic and admitting data was compared using a propensity score matched cohort. The cohort drawn from the ERCP and PTBD subcohorts and composed of a 1:1 unweighted match for age, sex, median household income, insurance, urban/rural location, and Charlson Comorbidity Index. Primary outcomes were readmission rates. Secondary outcomes included overall mortality, 30 day, 90 day and 6 month mortality, hospitalization cost, and length of stay. A Wilcoxon Two Sample test was conducted to assess significance for secondary outcomes, chi square test was conducted to assess primary outcomes, and Komogorov-Smirnov test was used to assess Charlson Comorbidity Index distribution.
Results: A total of 621,735 admissions were identified associated with 589,796 ERCP and 31,939 PTBD. In the propensity matched cohort, PTBD had a higher readmission rate at 30 days (20.38% vs 13.71% p< 0.0001), 90 days (14.63% vs 13.14%, p< 0.0001), but lower rate at 6 months (8.50% vs 9.67%, p=0.0003). Secondary outcomes included increased PTBD length of stay (9.01 days vs 6.74 days, p< 0.0001), hospitalization cost ($106,947.97 vs $97602.25, p< 0.0001), and overall mortality (6.86% vs 4.35%, p< 0.0001). No major differences were found for mortality among readmissions at 30 days (7.19% vs 6.88%, p=0.5382), 90 day (6.82% vs 6.51%, p=0.5612), and 6 months (5.08% vs 5.91%, p=0.1744).
Discussion: Although both ERCP and PTBD had no major differences in mortality among readmissions, patients who had ERCP had lower readmission rates, length of stay, and overall mortality. While ERCP may be associated with a health systems benefit in routine indications, a multi-disciplinary approach may be of benefit for complex cases.
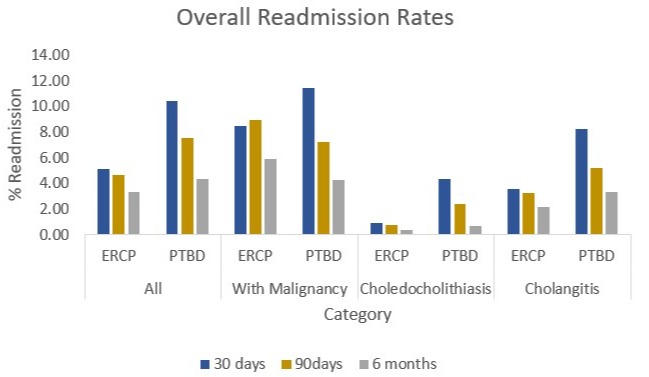
Figure: Figure 1. Overall readmission Rates Among Leading Procedure Indications Before Propensity Matching For ERCP Vs. PTBD In A National Cohort Between 2016-2020
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Daniel Wang indicated no relevant financial relationships.
Patrick Chang indicated no relevant financial relationships.
Supisara Tintara indicated no relevant financial relationships.
Frederick Chang indicated no relevant financial relationships.
Jennifer Phan indicated no relevant financial relationships.
Daniel Wang, MD1, Patrick Chang, MD2, Supisara Tintara, MD2, Frederick Chang, DO3, Jennifer Phan, MD2. P0070 - Comparative Analysis of ERCP and PTBD for Biliary Interventions for Readmission Rates and Patient Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
