Sunday Poster Session
Category: Biliary/Pancreas
P0124 - Post-Duodenal Polypectomy Pancreatitis: An Uncommon Iatrogenic Trigger
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Daniel A. Gonzalez Mosquera, MD
NYC Health + Hospitals/Lincoln
Bronx, NY
Presenting Author(s)
Daniel A. Gonzalez Mosquera, MD1, Rajiv Hans Menghrajani, MD2, Yassine Kilani, MD3, Marcus A. Banks, 4
1NYC Health + Hospitals/Lincoln, Bronx, NY; 2NYC Health + Hospitals/Lincoln, New York, NY; 3SSM Health Saint Louis University Hospital, St. Louis, MO; 4St. George's University School of Medicine, New York, NY
Introduction: Acute pancreatitis (AP) is a major cause of gastrointestinal-related admission in the United States, characterized by epigastric pain radiating to the back, and nausea and vomiting. Although commonly associated with alcohol consumption and gallstones, cases involving less frequent triggers, such as post-endoscopy, have been reported. We present an unusual case of post-polypectomy pancreatitis following esophagogastroduodenoscopy (EGD).
Case Description/Methods: A 20-year-old female, with a BMI of 45.9 kg/m² and a history of psychiatric disorders (including Anxiety, Depression, and Bipolar disorder), presented to the Emergency Department with severe epigastric and chest pain radiating to the back, three hours after a screening EGD for bariatric surgery, during which a duodenal polyp was resected. She developed nausea accompanied by severe epigastric and chest pain post-discharge, radiating to the back.
On initial evaluation, her vital signs included a temperature of 37°C, heart rate of 129/min, blood pressure of 105/95 mmHg, respiratory rate of 18/min, and 99% room air saturation. Physical examination revealed tenderness in the epigastric region. Review of laboratory showed elevated Lipase ( >600 U/L) and leukocytosis (17.09 x10(3)/mcL), normal triglycerides (98 mg/dL). Computed Tomography (CT) of the abdomen and pelvis with contrast resulted in pancreatic fat induration and fluid accumulation. An abdominal ultrasound confirmed the absence of gallstones and lack of biliary duct dilation in the gallbladder. The diagnosis of AP was confirmed based on the three diagnostic criteria (abdominal pain unequal from usual AP, an elevated serum lipase level three times above the normal threshold, and radiological imaging signs of pancreatitis).
Upon admission, the patient received IV fluids, pain management, and antibiotics. She improved, transitioning to oral intake and ambulation by day 5, with discharge on day 9, prescribed pain control, and instructions for monitoring alarm symptoms.
Discussion: While AP tends to be triggered by well-known reasons, this particular case highlights a distinctive iatrogenic trigger - duodenal polypectomy. Only a handful of similar cases have been documented. The duodenum's peculiar proximity to important pancreatic structures may result in mechanical injury or heat-induced pancreatic damage. The management, similar to typical acute pancreatitis care, underscores the importance of supportive measures.
Disclosures:
Daniel A. Gonzalez Mosquera, MD1, Rajiv Hans Menghrajani, MD2, Yassine Kilani, MD3, Marcus A. Banks, 4. P0124 - Post-Duodenal Polypectomy Pancreatitis: An Uncommon Iatrogenic Trigger, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1NYC Health + Hospitals/Lincoln, Bronx, NY; 2NYC Health + Hospitals/Lincoln, New York, NY; 3SSM Health Saint Louis University Hospital, St. Louis, MO; 4St. George's University School of Medicine, New York, NY
Introduction: Acute pancreatitis (AP) is a major cause of gastrointestinal-related admission in the United States, characterized by epigastric pain radiating to the back, and nausea and vomiting. Although commonly associated with alcohol consumption and gallstones, cases involving less frequent triggers, such as post-endoscopy, have been reported. We present an unusual case of post-polypectomy pancreatitis following esophagogastroduodenoscopy (EGD).
Case Description/Methods: A 20-year-old female, with a BMI of 45.9 kg/m² and a history of psychiatric disorders (including Anxiety, Depression, and Bipolar disorder), presented to the Emergency Department with severe epigastric and chest pain radiating to the back, three hours after a screening EGD for bariatric surgery, during which a duodenal polyp was resected. She developed nausea accompanied by severe epigastric and chest pain post-discharge, radiating to the back.
On initial evaluation, her vital signs included a temperature of 37°C, heart rate of 129/min, blood pressure of 105/95 mmHg, respiratory rate of 18/min, and 99% room air saturation. Physical examination revealed tenderness in the epigastric region. Review of laboratory showed elevated Lipase ( >600 U/L) and leukocytosis (17.09 x10(3)/mcL), normal triglycerides (98 mg/dL). Computed Tomography (CT) of the abdomen and pelvis with contrast resulted in pancreatic fat induration and fluid accumulation. An abdominal ultrasound confirmed the absence of gallstones and lack of biliary duct dilation in the gallbladder. The diagnosis of AP was confirmed based on the three diagnostic criteria (abdominal pain unequal from usual AP, an elevated serum lipase level three times above the normal threshold, and radiological imaging signs of pancreatitis).
Upon admission, the patient received IV fluids, pain management, and antibiotics. She improved, transitioning to oral intake and ambulation by day 5, with discharge on day 9, prescribed pain control, and instructions for monitoring alarm symptoms.
Discussion: While AP tends to be triggered by well-known reasons, this particular case highlights a distinctive iatrogenic trigger - duodenal polypectomy. Only a handful of similar cases have been documented. The duodenum's peculiar proximity to important pancreatic structures may result in mechanical injury or heat-induced pancreatic damage. The management, similar to typical acute pancreatitis care, underscores the importance of supportive measures.
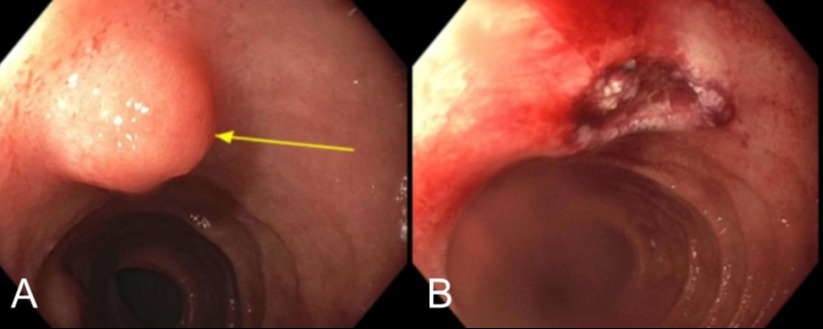
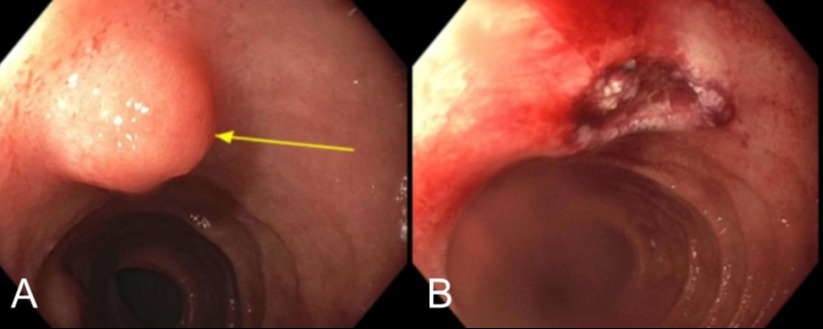
Figure: Figure 1. The screening esophagogastroduodenoscopy (EGD), shows a pedunculated polyp at the second portion of the duodenum proximal to the ampulla (A, see yellow arrow). Polypectomy was performed using a hot snare (B).
Disclosures:
Daniel Gonzalez Mosquera indicated no relevant financial relationships.
Rajiv Hans Menghrajani indicated no relevant financial relationships.
Yassine Kilani indicated no relevant financial relationships.
Marcus Banks indicated no relevant financial relationships.
Daniel A. Gonzalez Mosquera, MD1, Rajiv Hans Menghrajani, MD2, Yassine Kilani, MD3, Marcus A. Banks, 4. P0124 - Post-Duodenal Polypectomy Pancreatitis: An Uncommon Iatrogenic Trigger, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
