Sunday Poster Session
Category: Biliary/Pancreas
P0128 - Attack of the Clones: IgA-Induced Necrotizing Pancreatitis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Ryan Plunkett, MD
Saint Louis University School of Medicine
St. Louis, MO
Presenting Author(s)
Ryan Plunkett, MD1, Zain Raza, MD1, Jade Samanta, BS1, Neel Matiwala, BS1, Rohan Tripathi, BS1, Hayden Rotramel, MD2, Ameya Deshmukh, DO1, Brian Abboud, MD1, Jered Schenk, MD3, Tim Brotherton, MD2, Antonio R. Cheesman, MD2
1Saint Louis University School of Medicine, St. Louis, MO; 2SSM Health Saint Louis University Hospital, St. Louis, MO; 3Medical University of South Carolina, Charleston, SC
Introduction: IgA vasculitis (IgAV) is characterized by inflammation of the small blood vessels due to deposition of immunoglobulin A (IgA) immune complexes. Here, we highlight a case of IgA vasculitis where the patient developed a rare GI sequela, necrotizing pancreatitis.
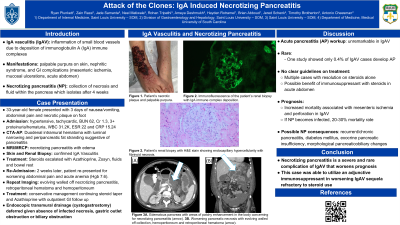
Case Description/Methods: A 33-year-old female presented with nausea, vomiting, and diffuse abdominal pain. Further examination revealed a necrotic right foot plaque and palpable purpura across her bilateral upper and lower extremities. On admission, notable labs included BUN 62, Cr 1.3, WBC 31,000, ESR 22, CRP 15, and 3+ proteinuria/hematuria. CTA-AP revealed an extensive duodenal intramural hematoma with luminal narrowing extending to the ligament of Treitz with additional findings of peripancreatic fat stranding suggestive of pancreatitis. MRI/MRCP confirmed severe necrotizing pancreatitis. IgAV was confirmed with renal and skin biopsies, specifically with renal biopsies demonstrating IgA immune complex deposition. No other identifiable risk factors for pancreatitis were identified. The stay was complicated by respiratory distress and diffuse alveolar hemorrhage. Steroids and azathioprine (AZA) were initiated, respiratory status and pain management greatly improved, and the patient was discharged. However, she was readmitted 2 weeks later with severe abdominal pain and emesis and was found to have evolving necrotizing pancreatitis with an evolving walled-off collection with a retroperitoneal hematoma and hemoperitoneum. This did not require endoscopic transmural drainage given the absence of infected necrosis, gastric outlet obstruction, or biliary obstruction. Management with steroids and AZA was continued and the patient was able to be discharged.
Discussion: There is a sparse number of documented cases describing patients with pancreatitis secondary to IgAV. In a retrospective single center study of 3212 IgAV patients, there were only 13 cases of clinically diagnosed AP between 2003 and 2016 (0.4%). Despite receiving appropriate treatment for IgAV, this patient still developed necrotizing pancreatitis, which highlights the importance of future research to identify clinical risk factors which may predict IgAV associated pancreatitis and determine optimal treatment strategies.

Disclosures:
Ryan Plunkett, MD1, Zain Raza, MD1, Jade Samanta, BS1, Neel Matiwala, BS1, Rohan Tripathi, BS1, Hayden Rotramel, MD2, Ameya Deshmukh, DO1, Brian Abboud, MD1, Jered Schenk, MD3, Tim Brotherton, MD2, Antonio R. Cheesman, MD2. P0128 - Attack of the Clones: IgA-Induced Necrotizing Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Saint Louis University School of Medicine, St. Louis, MO; 2SSM Health Saint Louis University Hospital, St. Louis, MO; 3Medical University of South Carolina, Charleston, SC
Introduction: IgA vasculitis (IgAV) is characterized by inflammation of the small blood vessels due to deposition of immunoglobulin A (IgA) immune complexes. Here, we highlight a case of IgA vasculitis where the patient developed a rare GI sequela, necrotizing pancreatitis.
Case Description/Methods: A 33-year-old female presented with nausea, vomiting, and diffuse abdominal pain. Further examination revealed a necrotic right foot plaque and palpable purpura across her bilateral upper and lower extremities. On admission, notable labs included BUN 62, Cr 1.3, WBC 31,000, ESR 22, CRP 15, and 3+ proteinuria/hematuria. CTA-AP revealed an extensive duodenal intramural hematoma with luminal narrowing extending to the ligament of Treitz with additional findings of peripancreatic fat stranding suggestive of pancreatitis. MRI/MRCP confirmed severe necrotizing pancreatitis. IgAV was confirmed with renal and skin biopsies, specifically with renal biopsies demonstrating IgA immune complex deposition. No other identifiable risk factors for pancreatitis were identified. The stay was complicated by respiratory distress and diffuse alveolar hemorrhage. Steroids and azathioprine (AZA) were initiated, respiratory status and pain management greatly improved, and the patient was discharged. However, she was readmitted 2 weeks later with severe abdominal pain and emesis and was found to have evolving necrotizing pancreatitis with an evolving walled-off collection with a retroperitoneal hematoma and hemoperitoneum. This did not require endoscopic transmural drainage given the absence of infected necrosis, gastric outlet obstruction, or biliary obstruction. Management with steroids and AZA was continued and the patient was able to be discharged.
Discussion: There is a sparse number of documented cases describing patients with pancreatitis secondary to IgAV. In a retrospective single center study of 3212 IgAV patients, there were only 13 cases of clinically diagnosed AP between 2003 and 2016 (0.4%). Despite receiving appropriate treatment for IgAV, this patient still developed necrotizing pancreatitis, which highlights the importance of future research to identify clinical risk factors which may predict IgAV associated pancreatitis and determine optimal treatment strategies.

Figure: Figure 1. Edematous pancreas with non-enhancement of the majority of the pancreas with areas of patchy enhancement of the body concerning for necrotizing pancreatitis.
Disclosures:
Ryan Plunkett indicated no relevant financial relationships.
Zain Raza indicated no relevant financial relationships.
Jade Samanta indicated no relevant financial relationships.
Neel Matiwala indicated no relevant financial relationships.
Rohan Tripathi indicated no relevant financial relationships.
Hayden Rotramel indicated no relevant financial relationships.
Ameya Deshmukh indicated no relevant financial relationships.
Brian Abboud indicated no relevant financial relationships.
Jered Schenk indicated no relevant financial relationships.
Tim Brotherton indicated no relevant financial relationships.
Antonio Cheesman indicated no relevant financial relationships.
Ryan Plunkett, MD1, Zain Raza, MD1, Jade Samanta, BS1, Neel Matiwala, BS1, Rohan Tripathi, BS1, Hayden Rotramel, MD2, Ameya Deshmukh, DO1, Brian Abboud, MD1, Jered Schenk, MD3, Tim Brotherton, MD2, Antonio R. Cheesman, MD2. P0128 - Attack of the Clones: IgA-Induced Necrotizing Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
