Sunday Poster Session
Category: Biliary/Pancreas
P0133 - Pancreatitis Fooling Doctors and Masquerading a Large Hemoperitoneum due to a Rare Pancreaticoduodenal Artery Aneurysm
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Saadia Nabi, MD
Aventura Hospital
Aventura, FL
Presenting Author(s)
Ambar Sekulits, MD1, Saadia Nabi, MD2, Luis Santiago, MD2, Francini Alcocer, MD2, Sinay Ceballos, MD2, Rafael Miret, DO2, Raiko Diaz, DO2
1Aventura Hospital, Dania Beach, FL; 2Aventura Hospital, Aventura, FL
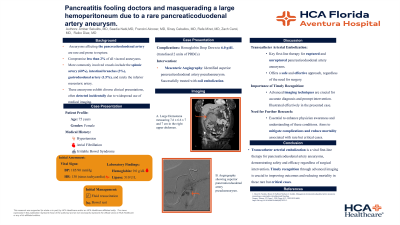
Introduction: Aneurysms affecting the pancreaticoduodenal artery are rare and prone to rupture, comprising less than 2% of all visceral aneurysms. Approximately 100 cases have been reported in literature review, with diameters typically ranging from 0.7 to 1.2 cm. More commonly involved vessels include the splenic artery (60%), intestinal branches (3%), gastroduodenal artery (1.5%), and rarely the inferior mesenteric artery. These aneurysms exhibit diverse clinical presentations, often detected incidentally due to widespread use of medical imaging. Here we discuss a case of pancreatitis masking a large hemoperitoneum from a pancreaticoduodenal artery aneurysm.
Case Description/Methods: A 75-year-old female with a significant medical history of hypertension, atrial fibrillation, and irritable bowel syndrome presented to the hospital with epigastric pain radiating to the back, accompanied by generalized weakness and pale stools ongoing for 3 days. On arrival, her blood pressure was elevated at 185/90 mmHg, with other vital signs within normal limits. Laboratory findings revealed a hemoglobin level of 9.0 g/dL, minimal leukocytosis (12.9 x 10^9/L), and a lipase level of 510 U/L. Treatment was initiated promptly based on the presence of classic pancreatitis findings, including fluid resuscitation and bowel rest. As there was no improvement in symptoms a subsequent abdominal CT scan identified a large 7.6 cm x 6 cm x 7 cm soft tissue density mass indicative of a significant peritoneal hematoma. Overnight, the patient's hemoglobin dropped to 6.0 g/dL, necessitating transfusion of 2 units of packed red blood cells. A repeat CT showed worsening hemoperitoneum, prompting urgent mesenteric angiography. This revealed a superior pancreaticoduodenal artery pseudoaneurysm, successfully treated with coil embolization. The patient recovered and was discharged two days later without complications.
Discussion: In conclusion, transcatheter arterial embolization emerges as a pivotal first-line therapy for both ruptured and unruptured pancreaticoduodenal artery aneurysms, offering a safe and effective approach whether surgery is ultimately required or not. Timely recognition through advanced imaging techniques is crucial for accurate diagnosis and prompt intervention, as illustrated by the case presented here. Further research is essential to enhance physician awareness, mitigate complications, and reduce mortality associated with these rare but critical cases.
Disclosures:
Ambar Sekulits, MD1, Saadia Nabi, MD2, Luis Santiago, MD2, Francini Alcocer, MD2, Sinay Ceballos, MD2, Rafael Miret, DO2, Raiko Diaz, DO2. P0133 - Pancreatitis Fooling Doctors and Masquerading a Large Hemoperitoneum due to a Rare Pancreaticoduodenal Artery Aneurysm, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Aventura Hospital, Dania Beach, FL; 2Aventura Hospital, Aventura, FL
Introduction: Aneurysms affecting the pancreaticoduodenal artery are rare and prone to rupture, comprising less than 2% of all visceral aneurysms. Approximately 100 cases have been reported in literature review, with diameters typically ranging from 0.7 to 1.2 cm. More commonly involved vessels include the splenic artery (60%), intestinal branches (3%), gastroduodenal artery (1.5%), and rarely the inferior mesenteric artery. These aneurysms exhibit diverse clinical presentations, often detected incidentally due to widespread use of medical imaging. Here we discuss a case of pancreatitis masking a large hemoperitoneum from a pancreaticoduodenal artery aneurysm.
Case Description/Methods: A 75-year-old female with a significant medical history of hypertension, atrial fibrillation, and irritable bowel syndrome presented to the hospital with epigastric pain radiating to the back, accompanied by generalized weakness and pale stools ongoing for 3 days. On arrival, her blood pressure was elevated at 185/90 mmHg, with other vital signs within normal limits. Laboratory findings revealed a hemoglobin level of 9.0 g/dL, minimal leukocytosis (12.9 x 10^9/L), and a lipase level of 510 U/L. Treatment was initiated promptly based on the presence of classic pancreatitis findings, including fluid resuscitation and bowel rest. As there was no improvement in symptoms a subsequent abdominal CT scan identified a large 7.6 cm x 6 cm x 7 cm soft tissue density mass indicative of a significant peritoneal hematoma. Overnight, the patient's hemoglobin dropped to 6.0 g/dL, necessitating transfusion of 2 units of packed red blood cells. A repeat CT showed worsening hemoperitoneum, prompting urgent mesenteric angiography. This revealed a superior pancreaticoduodenal artery pseudoaneurysm, successfully treated with coil embolization. The patient recovered and was discharged two days later without complications.
Discussion: In conclusion, transcatheter arterial embolization emerges as a pivotal first-line therapy for both ruptured and unruptured pancreaticoduodenal artery aneurysms, offering a safe and effective approach whether surgery is ultimately required or not. Timely recognition through advanced imaging techniques is crucial for accurate diagnosis and prompt intervention, as illustrated by the case presented here. Further research is essential to enhance physician awareness, mitigate complications, and reduce mortality associated with these rare but critical cases.
Disclosures:
Ambar Sekulits indicated no relevant financial relationships.
Saadia Nabi indicated no relevant financial relationships.
Luis Santiago indicated no relevant financial relationships.
Francini Alcocer indicated no relevant financial relationships.
Sinay Ceballos indicated no relevant financial relationships.
Rafael Miret indicated no relevant financial relationships.
Raiko Diaz indicated no relevant financial relationships.
Ambar Sekulits, MD1, Saadia Nabi, MD2, Luis Santiago, MD2, Francini Alcocer, MD2, Sinay Ceballos, MD2, Rafael Miret, DO2, Raiko Diaz, DO2. P0133 - Pancreatitis Fooling Doctors and Masquerading a Large Hemoperitoneum due to a Rare Pancreaticoduodenal Artery Aneurysm, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
