Sunday Poster Session
Category: Biliary/Pancreas
P0138 - Acute Pancreatitis Secondary to Olanzapine-Induced Hypertriglyceridemia: A Case Report
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- SZ
Syed Muhammad Hussain Zaidi, MD
The Wright Center for Community Health
Scranton, PA
Presenting Author(s)
Udit Asija, MD1, Syed Muhammad Hussain Zaidi, MD2, Kanishq Jethani, MD2, Muhammad Hassan Shakir, MD2, Fatima Tanveer, 2, Salman Abdul Basit, MD2, Muhammad Waqas, MD3, Mina Daniel, 2, Peter Iskander, MD2, Mohammed Taraqul Khan, 2, Qi Shi, MD4
1The Wright Center for Graduate Medical Education, Scranton, PA; 2The Wright Center for Community Health, Scranton, PA; 3Wright Center for Graduate Medical Education, Scranton, PA; 4Geisinger Community Medical Center, Scranton, PA
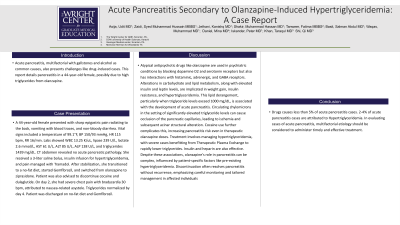
Introduction: Acute pancreatitis, multifactorial with gallstones and alcohol as common causes, also presents challenges like drug-induced cases. This report details pancreatitis in a 44-year-old female, possibly due to high triglycerides from olanzapine.
Case Description/Methods: A 44-year-old female presented with sharp epigastric pain radiating to the back, vomiting with blood traces, and non-bloody diarrhea. Vital signs included a temperature of 99.1°F, BP 150/93 mmHg, HR 115 bpm, RR 16/min. Labs showed WBC 13.25 K/uL, lipase 239 U/L, lactate 2.6 mmol/L, AST 61 U/L, ALT 85 U/L, ALP 138 U/L, and triglycerides 1439 mg/dL. CT abdomen revealed no acute pancreatic pathology. She received a 3-liter saline bolus, insulin infusion for hypertriglyceridemia, and pain managed with Tramadol. After stabilization, she transitioned to a no-fat diet, started Gemfibrozil, and switched from olanzapine to ziprasidone. Patient was also advised to discontinue cocaine and dulaglutide. On day 2, she had severe chest pain with bradycardia 30 bpm, attributed to nausea-related asystole. Triglycerides normalized by day 4. Patient was discharged on no-fat diet and Gemfibrozil.
Discussion: Atypical antipsychotic drugs like olanzapine are used in psychiatric conditions by blocking dopamine D2 and serotonin receptors but also has interactions with histaminic, adrenergic, and GABA receptors. Alterations in carbohydrate and lipid metabolism, along with elevated insulin and leptin levels, are implicated in weight gain, insulin resistance, and hypertriglyceridemia. This lipid derangement, particularly when triglyceride levels exceed 1000 mg/dL, is associated with the development of acute pancreatitis. Circulating chylomicrons in the setting of significantly elevated triglyceride levels can cause occlusion of the pancreatic capillaries, leading to ischemia and subsequent acinar structural alteration. Cocaine use further complicates this, increasing pancreatitis risk even in therapeutic olanzapine doses. Treatment involves managing hypertriglyceridemia, with severe cases benefitting from Therapeutic Plasma Exchange to rapidly lower triglycerides. Insulin and heparin are also effective. Despite these associations, olanzapine's role in pancreatitis can be complex, influenced by patient-specific factors like pre-existing hypertriglyceridemia. Discontinuation often resolves pancreatitis without recurrence, emphasizing careful monitoring and tailored management in affected individuals.
Disclosures:
Udit Asija, MD1, Syed Muhammad Hussain Zaidi, MD2, Kanishq Jethani, MD2, Muhammad Hassan Shakir, MD2, Fatima Tanveer, 2, Salman Abdul Basit, MD2, Muhammad Waqas, MD3, Mina Daniel, 2, Peter Iskander, MD2, Mohammed Taraqul Khan, 2, Qi Shi, MD4. P0138 - Acute Pancreatitis Secondary to Olanzapine-Induced Hypertriglyceridemia: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1The Wright Center for Graduate Medical Education, Scranton, PA; 2The Wright Center for Community Health, Scranton, PA; 3Wright Center for Graduate Medical Education, Scranton, PA; 4Geisinger Community Medical Center, Scranton, PA
Introduction: Acute pancreatitis, multifactorial with gallstones and alcohol as common causes, also presents challenges like drug-induced cases. This report details pancreatitis in a 44-year-old female, possibly due to high triglycerides from olanzapine.
Case Description/Methods: A 44-year-old female presented with sharp epigastric pain radiating to the back, vomiting with blood traces, and non-bloody diarrhea. Vital signs included a temperature of 99.1°F, BP 150/93 mmHg, HR 115 bpm, RR 16/min. Labs showed WBC 13.25 K/uL, lipase 239 U/L, lactate 2.6 mmol/L, AST 61 U/L, ALT 85 U/L, ALP 138 U/L, and triglycerides 1439 mg/dL. CT abdomen revealed no acute pancreatic pathology. She received a 3-liter saline bolus, insulin infusion for hypertriglyceridemia, and pain managed with Tramadol. After stabilization, she transitioned to a no-fat diet, started Gemfibrozil, and switched from olanzapine to ziprasidone. Patient was also advised to discontinue cocaine and dulaglutide. On day 2, she had severe chest pain with bradycardia 30 bpm, attributed to nausea-related asystole. Triglycerides normalized by day 4. Patient was discharged on no-fat diet and Gemfibrozil.
Discussion: Atypical antipsychotic drugs like olanzapine are used in psychiatric conditions by blocking dopamine D2 and serotonin receptors but also has interactions with histaminic, adrenergic, and GABA receptors. Alterations in carbohydrate and lipid metabolism, along with elevated insulin and leptin levels, are implicated in weight gain, insulin resistance, and hypertriglyceridemia. This lipid derangement, particularly when triglyceride levels exceed 1000 mg/dL, is associated with the development of acute pancreatitis. Circulating chylomicrons in the setting of significantly elevated triglyceride levels can cause occlusion of the pancreatic capillaries, leading to ischemia and subsequent acinar structural alteration. Cocaine use further complicates this, increasing pancreatitis risk even in therapeutic olanzapine doses. Treatment involves managing hypertriglyceridemia, with severe cases benefitting from Therapeutic Plasma Exchange to rapidly lower triglycerides. Insulin and heparin are also effective. Despite these associations, olanzapine's role in pancreatitis can be complex, influenced by patient-specific factors like pre-existing hypertriglyceridemia. Discontinuation often resolves pancreatitis without recurrence, emphasizing careful monitoring and tailored management in affected individuals.
Disclosures:
Udit Asija indicated no relevant financial relationships.
Syed Muhammad Hussain Zaidi indicated no relevant financial relationships.
Kanishq Jethani indicated no relevant financial relationships.
Muhammad Hassan Shakir indicated no relevant financial relationships.
Fatima Tanveer indicated no relevant financial relationships.
Salman Abdul Basit indicated no relevant financial relationships.
Muhammad Waqas indicated no relevant financial relationships.
Mina Daniel indicated no relevant financial relationships.
Peter Iskander indicated no relevant financial relationships.
Mohammed Taraqul Khan indicated no relevant financial relationships.
Qi Shi indicated no relevant financial relationships.
Udit Asija, MD1, Syed Muhammad Hussain Zaidi, MD2, Kanishq Jethani, MD2, Muhammad Hassan Shakir, MD2, Fatima Tanveer, 2, Salman Abdul Basit, MD2, Muhammad Waqas, MD3, Mina Daniel, 2, Peter Iskander, MD2, Mohammed Taraqul Khan, 2, Qi Shi, MD4. P0138 - Acute Pancreatitis Secondary to Olanzapine-Induced Hypertriglyceridemia: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
