Sunday Poster Session
Category: Biliary/Pancreas
P0140 - Unanticipated Culprits: A Rare Case of Drug-Induced Acute Necrotizing Pancreatitis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- KB
Kirsten Brinkmeier, BS
Wayne State University School of Medicine
Detroit, MI
Presenting Author(s)
Jacob Waitzman, BS1, Kirsten Brinkmeier, BS2, Majd Khadra, MD3, Kenan Abou Chaer, MD3, Brianna P.. Desa, DO3, Kamalakar Nerusu, MD3
1Wayne State University School of Medicine, Franklin, MI; 2Wayne State University School of Medicine, Detroit, MI; 3Detroit Medical Center, Detroit, MI
Introduction: Acute pancreatitis (AP) is the most common gastrointestinal condition requiring hospitalization in the U.S., with increasing prevalence year-to-year. Patients typically present with epigastric or diffuse abdominal pain radiating to the back. Common causes include gallstones, alcohol use, hypertriglyceridemia, and prescription drugs. Acute necrotizing pancreatitis (ANP) is a severe complication involving pancreatic tissue necrosis, with a mortality rate of 3% for mild AP and up to 20% for ANP. About 33% of ANP cases develop infected necrosis, significantly increasing mortality.
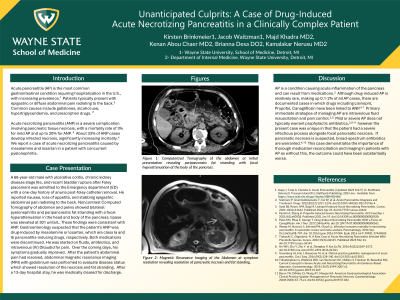
Case Description/Methods: A 68 year old male with ulcerative colitis, chronic kidney disease stage IIIa, and recent bladder rupture after Foley placement was admitted to the Emergency department (ED) with a one day history of anuria post-foley catheter removal. He reported nausea, loss of appetite, and stabbing epigastric abdominal pain radiating to the back. Noncontrast Computed Tomography of abdomen and pelvis showed bilateral pyelonephritis and peripancreatic fat stranding with a focal hyperattenuation in the head and body of the pancreas; lipase was elevated at 301 units/L. These findings were consistent with ANP. Gastroenterology suspected that the patient’s ANP was drug-induced by mesalamine or losartan, which are class Ia and Ib pancreatitis-inducing drugs, respectively. Both of these medications were discontinued. He was started on fluids, antibiotics, and intravenous (IV) Dilaudid for pain. Over the coming days, his symptoms gradually improved. After the patient’s abdominal pain had resolved, abdominal magnetic resonance imaging (MRI) with gadolinium was performed to evaluate disease status which showed resolution of the necrosis and fat stranding. After a 13 day hospital stay, he was medically cleared for discharge.
Discussion: This case highlights the importance of considering acute necrotizing pancreatitis in patients receiving mesalamine or losartan who present with epigastric abdominal pain. Additionally, it is important to note that while antibiotics are typically not warranted in the management of AP, this was an unusual case in which a concurrent infectious process was present and preventing infected necrosis of the pancreas was of utmost importance. Early recognition, cessation of the suspected medications, and appropriate management are crucial in achieving favorable outcomes and preventing further complications in such individuals.

Disclosures:
Jacob Waitzman, BS1, Kirsten Brinkmeier, BS2, Majd Khadra, MD3, Kenan Abou Chaer, MD3, Brianna P.. Desa, DO3, Kamalakar Nerusu, MD3. P0140 - Unanticipated Culprits: A Rare Case of Drug-Induced Acute Necrotizing Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Wayne State University School of Medicine, Franklin, MI; 2Wayne State University School of Medicine, Detroit, MI; 3Detroit Medical Center, Detroit, MI
Introduction: Acute pancreatitis (AP) is the most common gastrointestinal condition requiring hospitalization in the U.S., with increasing prevalence year-to-year. Patients typically present with epigastric or diffuse abdominal pain radiating to the back. Common causes include gallstones, alcohol use, hypertriglyceridemia, and prescription drugs. Acute necrotizing pancreatitis (ANP) is a severe complication involving pancreatic tissue necrosis, with a mortality rate of 3% for mild AP and up to 20% for ANP. About 33% of ANP cases develop infected necrosis, significantly increasing mortality.
Case Description/Methods: A 68 year old male with ulcerative colitis, chronic kidney disease stage IIIa, and recent bladder rupture after Foley placement was admitted to the Emergency department (ED) with a one day history of anuria post-foley catheter removal. He reported nausea, loss of appetite, and stabbing epigastric abdominal pain radiating to the back. Noncontrast Computed Tomography of abdomen and pelvis showed bilateral pyelonephritis and peripancreatic fat stranding with a focal hyperattenuation in the head and body of the pancreas; lipase was elevated at 301 units/L. These findings were consistent with ANP. Gastroenterology suspected that the patient’s ANP was drug-induced by mesalamine or losartan, which are class Ia and Ib pancreatitis-inducing drugs, respectively. Both of these medications were discontinued. He was started on fluids, antibiotics, and intravenous (IV) Dilaudid for pain. Over the coming days, his symptoms gradually improved. After the patient’s abdominal pain had resolved, abdominal magnetic resonance imaging (MRI) with gadolinium was performed to evaluate disease status which showed resolution of the necrosis and fat stranding. After a 13 day hospital stay, he was medically cleared for discharge.
Discussion: This case highlights the importance of considering acute necrotizing pancreatitis in patients receiving mesalamine or losartan who present with epigastric abdominal pain. Additionally, it is important to note that while antibiotics are typically not warranted in the management of AP, this was an unusual case in which a concurrent infectious process was present and preventing infected necrosis of the pancreas was of utmost importance. Early recognition, cessation of the suspected medications, and appropriate management are crucial in achieving favorable outcomes and preventing further complications in such individuals.

Figure: Focal area of necrosis in pancreatic body and head.
Disclosures:
Jacob Waitzman indicated no relevant financial relationships.
Kirsten Brinkmeier indicated no relevant financial relationships.
Majd Khadra indicated no relevant financial relationships.
Kenan Abou Chaer indicated no relevant financial relationships.
Brianna Desa indicated no relevant financial relationships.
Kamalakar Nerusu indicated no relevant financial relationships.
Jacob Waitzman, BS1, Kirsten Brinkmeier, BS2, Majd Khadra, MD3, Kenan Abou Chaer, MD3, Brianna P.. Desa, DO3, Kamalakar Nerusu, MD3. P0140 - Unanticipated Culprits: A Rare Case of Drug-Induced Acute Necrotizing Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
