Sunday Poster Session
Category: Biliary/Pancreas
P0144 - Left Breathless: Tension Hydrothorax Caused by a Pancreaticopleural Fistula
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Amanda Frondella, MD
UConn John Dempsey Hospital
Farmington, CT
Presenting Author(s)
Amanda Frondella, MD1, Geraldine N.. Nabeta, MD1, Minh Thu T.. Nguyen, MD2, Courtenay Ryan-Fisher, MBBCh2, Lisa Rossi, MD3
1UConn John Dempsey Hospital, Farmington, CT; 2University of Connecticut Health Center, Farmington, CT; 3University of Connecticut Health Center, Hartford, CT
Introduction: Pancreaticopleural fistula (PPF), a rare complication of pancreatitis, poses life-threatening risks. Elevated amylase levels in pleural fluid warrant prompt imaging and intervention. Here, we present a case of right tension hydrothorax caused by a PPF.
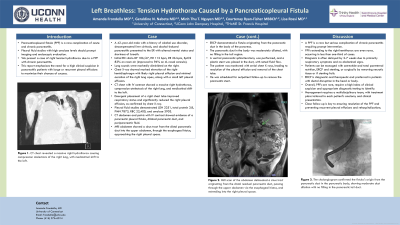
Case Description/Methods: A 42-year-old male with decompensated alcoholic cirrhosis, prior hepatic encephalopathy, and chronic pancreatitis presented with altered mentation and dyspnea. Vital signs were BP 106/67, HR 112 bpm, RR 26 bpm, and SpO2 83% on room air (improved to 96% on 4L O2 NC). Diminished lung sounds were noted on the right side. CT chest revealed a massive right hydrothorax causing compression atelectasis of the right lung, with mediastinal shift to the left (Figure 1a). Emergent chest tube insertion led to improved respiratory status and reduction in pleural effusion. Pleural fluid studies showed LDH 2,251, total protein 3.8, PMN 7,873, RBC 22,400, and amylase 3,903.
CT abdomen and subsequent MRI abdomen scans delineated a sinus tract originating from the distal residual pancreatic duct, traversing the upper abdomen through the esophageal hiatus, and reaching the right pleural space (Figure 1b). ERCP confirmed the fistula's origin from the pancreatic duct in the pancreatic body, with moderate duct dilation and no duct filling of the pancreatic tail (Figure 1c). Following a pancreatic sphincterotomy, a plastic stent was placed in the ventral pancreatic duct to facilitate flow. Eventually, the pleural effusion resolved, and the chest tube was removed. The patient is scheduled for outpatient ERCP for stent removal.
Discussion: A PPF is a rare yet serious complication of chronic pancreatitis. PPFs extending to the right hemithorax are even rarer, occurring in less than one-third of cases. Diagnosis is often delayed by up to 2-7 weeks as symptoms primarily manifest as respiratory issues with no associated abdominal pain. These patients can be managed medically with octreotide and total parenteral nutrition, endoscopically with ERCP and stent placement, or surgically by removing necrotic pancreatic tissue or addressing fistula closure failure with stenting. ERCP serves as both a diagnostic and therapeutic tool and is preferred in patients with ductal disruption in the head or body, as observed in our case. Close follow-up is essential to ensure PPF resolution. This case underscores the importance of maintaining clinical suspicion in patients with pancreatitis presenting with large or recurrent unilateral pleural effusions.
Disclosures:
Amanda Frondella, MD1, Geraldine N.. Nabeta, MD1, Minh Thu T.. Nguyen, MD2, Courtenay Ryan-Fisher, MBBCh2, Lisa Rossi, MD3. P0144 - Left Breathless: Tension Hydrothorax Caused by a Pancreaticopleural Fistula, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1UConn John Dempsey Hospital, Farmington, CT; 2University of Connecticut Health Center, Farmington, CT; 3University of Connecticut Health Center, Hartford, CT
Introduction: Pancreaticopleural fistula (PPF), a rare complication of pancreatitis, poses life-threatening risks. Elevated amylase levels in pleural fluid warrant prompt imaging and intervention. Here, we present a case of right tension hydrothorax caused by a PPF.
Case Description/Methods: A 42-year-old male with decompensated alcoholic cirrhosis, prior hepatic encephalopathy, and chronic pancreatitis presented with altered mentation and dyspnea. Vital signs were BP 106/67, HR 112 bpm, RR 26 bpm, and SpO2 83% on room air (improved to 96% on 4L O2 NC). Diminished lung sounds were noted on the right side. CT chest revealed a massive right hydrothorax causing compression atelectasis of the right lung, with mediastinal shift to the left (Figure 1a). Emergent chest tube insertion led to improved respiratory status and reduction in pleural effusion. Pleural fluid studies showed LDH 2,251, total protein 3.8, PMN 7,873, RBC 22,400, and amylase 3,903.
CT abdomen and subsequent MRI abdomen scans delineated a sinus tract originating from the distal residual pancreatic duct, traversing the upper abdomen through the esophageal hiatus, and reaching the right pleural space (Figure 1b). ERCP confirmed the fistula's origin from the pancreatic duct in the pancreatic body, with moderate duct dilation and no duct filling of the pancreatic tail (Figure 1c). Following a pancreatic sphincterotomy, a plastic stent was placed in the ventral pancreatic duct to facilitate flow. Eventually, the pleural effusion resolved, and the chest tube was removed. The patient is scheduled for outpatient ERCP for stent removal.
Discussion: A PPF is a rare yet serious complication of chronic pancreatitis. PPFs extending to the right hemithorax are even rarer, occurring in less than one-third of cases. Diagnosis is often delayed by up to 2-7 weeks as symptoms primarily manifest as respiratory issues with no associated abdominal pain. These patients can be managed medically with octreotide and total parenteral nutrition, endoscopically with ERCP and stent placement, or surgically by removing necrotic pancreatic tissue or addressing fistula closure failure with stenting. ERCP serves as both a diagnostic and therapeutic tool and is preferred in patients with ductal disruption in the head or body, as observed in our case. Close follow-up is essential to ensure PPF resolution. This case underscores the importance of maintaining clinical suspicion in patients with pancreatitis presenting with large or recurrent unilateral pleural effusions.
Figure: Figure 1a) The CT chest showed a large right hydrothorax leading to compression atelectasis of the right lung, accompanied by mediastinal displacement to the left. b) MRI scan of the abdomen delineated a sinus tract originating from the distal residual pancreatic duct, passing through the upper abdomen via the esophageal hiatus, and extending into the right pleural space. c) The cholangiogram confirmed the fistula's origin from the pancreatic duct in the pancreatic body, showing moderate duct dilation with no filling in the pancreatic tail duct.
Disclosures:
Amanda Frondella indicated no relevant financial relationships.
Geraldine Nabeta indicated no relevant financial relationships.
Minh Thu Nguyen indicated no relevant financial relationships.
Courtenay Ryan-Fisher indicated no relevant financial relationships.
Lisa Rossi indicated no relevant financial relationships.
Amanda Frondella, MD1, Geraldine N.. Nabeta, MD1, Minh Thu T.. Nguyen, MD2, Courtenay Ryan-Fisher, MBBCh2, Lisa Rossi, MD3. P0144 - Left Breathless: Tension Hydrothorax Caused by a Pancreaticopleural Fistula, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
