Sunday Poster Session
Category: Biliary/Pancreas
P0171 - Silent Hemorrhage: Hemorrhagic Pancreatitis Without Systemic Shock
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Panida Charnvitayapong, MD
University of Miami Miller School of Medicine at JFK Medical Center
Lantana, FL
Presenting Author(s)
Panida Charnvitayapong, MD1, Michelle Cheung, DO2, Lesley Ann Mccook, MD2, Stefanie Furlan, DO2
1University of Miami Miller School of Medicine at JFK Medical Center, Lantana, FL; 2University of Miami Miller School of Medicine at JFK Medical Center, Atlantis, FL
Introduction: Hemorrhagic pancreatitis, a severe form of acute pancreatitis, involves bleeding within or around the pancreas and typically presents with hemodynamic instability and systemic complications. Atypical presentations without systemic shock are underreported. This case highlights the variability in hemorrhagic pancreatitis presentation and the importance of thorough diagnostic evaluation.
Case Description/Methods: A 55-year-old male with a history of extensive alcohol and opioid use, a family history of pancreatic cancer, hypertension, and hiatal hernia presented with severe periumbilical and epigastric abdominal pain rated 10/10 starting the night before admission. He had been in detox recovery for a month and had no history of gallstone disease or prior pancreatitis episodes. The pain was unrelieved by any measures.
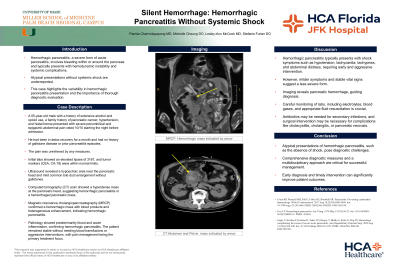
Initial labs showed an elevated lipase of 3167, and tumor markers (CEA, CA-19) were within normal limits. Ultrasound revealed a hypoechoic area near the pancreatic head and mild common bile duct enlargement without gallstones. Computed tomography (CT) scan showed a hyperdense mass at the pancreatic head, suggesting hemorrhagic pancreatitis or a hemorrhaged pancreatic mass. Magnetic resonance cholangiopancreatography (MRCP) confirmed a hemorrhagic mass with blood products and heterogeneous enhancement, indicating hemorrhagic pancreatitis. Pathology showed predominantly blood and acute inflammation, confirming hemorrhagic pancreatitis. The patient remained stable without needing blood transfusions or aggressive interventions, with pain management being the primary treatment focus.
Discussion: Hemorrhagic pancreatitis typically presents with shock symptoms such as hypotension, tachycardia, tachypnea, and abdominal distress, requiring early and aggressive intervention. However, milder symptoms and stable vital signs suggest a less severe form. Imaging reveals pancreatic hemorrhage, guiding diagnosis. Careful monitoring of labs, including electrolytes, blood gases, and appropriate fluid resuscitation is crucial. Antibiotics may be needed for secondary infections, and surgical intervention may be necessary for complications like cholecystitis, cholangitis, or pancreatic necrosis.
Atypical presentations of hemorrhagic pancreatitis, such as the absence of shock, pose diagnostic challenges. Comprehensive diagnostic measures and a multidisciplinary approach are critical for successful management. Early diagnosis and timely intervention can significantly improve patient outcomes.
Disclosures:
Panida Charnvitayapong, MD1, Michelle Cheung, DO2, Lesley Ann Mccook, MD2, Stefanie Furlan, DO2. P0171 - Silent Hemorrhage: Hemorrhagic Pancreatitis Without Systemic Shock, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Miami Miller School of Medicine at JFK Medical Center, Lantana, FL; 2University of Miami Miller School of Medicine at JFK Medical Center, Atlantis, FL
Introduction: Hemorrhagic pancreatitis, a severe form of acute pancreatitis, involves bleeding within or around the pancreas and typically presents with hemodynamic instability and systemic complications. Atypical presentations without systemic shock are underreported. This case highlights the variability in hemorrhagic pancreatitis presentation and the importance of thorough diagnostic evaluation.
Case Description/Methods: A 55-year-old male with a history of extensive alcohol and opioid use, a family history of pancreatic cancer, hypertension, and hiatal hernia presented with severe periumbilical and epigastric abdominal pain rated 10/10 starting the night before admission. He had been in detox recovery for a month and had no history of gallstone disease or prior pancreatitis episodes. The pain was unrelieved by any measures.
Initial labs showed an elevated lipase of 3167, and tumor markers (CEA, CA-19) were within normal limits. Ultrasound revealed a hypoechoic area near the pancreatic head and mild common bile duct enlargement without gallstones. Computed tomography (CT) scan showed a hyperdense mass at the pancreatic head, suggesting hemorrhagic pancreatitis or a hemorrhaged pancreatic mass. Magnetic resonance cholangiopancreatography (MRCP) confirmed a hemorrhagic mass with blood products and heterogeneous enhancement, indicating hemorrhagic pancreatitis. Pathology showed predominantly blood and acute inflammation, confirming hemorrhagic pancreatitis. The patient remained stable without needing blood transfusions or aggressive interventions, with pain management being the primary treatment focus.
Discussion: Hemorrhagic pancreatitis typically presents with shock symptoms such as hypotension, tachycardia, tachypnea, and abdominal distress, requiring early and aggressive intervention. However, milder symptoms and stable vital signs suggest a less severe form. Imaging reveals pancreatic hemorrhage, guiding diagnosis. Careful monitoring of labs, including electrolytes, blood gases, and appropriate fluid resuscitation is crucial. Antibiotics may be needed for secondary infections, and surgical intervention may be necessary for complications like cholecystitis, cholangitis, or pancreatic necrosis.
Atypical presentations of hemorrhagic pancreatitis, such as the absence of shock, pose diagnostic challenges. Comprehensive diagnostic measures and a multidisciplinary approach are critical for successful management. Early diagnosis and timely intervention can significantly improve patient outcomes.
Disclosures:
Panida Charnvitayapong indicated no relevant financial relationships.
Michelle Cheung indicated no relevant financial relationships.
Lesley Ann Mccook indicated no relevant financial relationships.
Stefanie Furlan indicated no relevant financial relationships.
Panida Charnvitayapong, MD1, Michelle Cheung, DO2, Lesley Ann Mccook, MD2, Stefanie Furlan, DO2. P0171 - Silent Hemorrhage: Hemorrhagic Pancreatitis Without Systemic Shock, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
