Sunday Poster Session
Category: Biliary/Pancreas
P0172 - Unusual Cause of Hematochezia in a Patient With Metastatic Gallbladder Carcinoma: A Case Report and Review of Literature
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Mannat Kaur Bhatia, MD
Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School
New Brunswick, NJ
Presenting Author(s)
Mannat Kaur. Bhatia, MD, Luisa Recinos, MD, Sugirdhana Velpari, MD
Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ
Introduction: Gallbladder carcinoma (GBC) is a rare and aggressive biliary tract malignancy often mimicking benign disease, leading to delayed diagnosis and poor prognosis. The reported 5-year survival rates are 80% (stage 0), 50% (stage I), 28% (stage II), and < 10% (stages III-IV). While most GBC cases are discovered incidentally and metastasis can occur through direct invasion, peritoneal dissemination, or hematogenous dissemination, metastasis to the colon is exceedingly rare. This report presents a unique case of GBC with direct invasion into the colon, detailing endoscopic, computed tomography (CT), and histopathological findings.
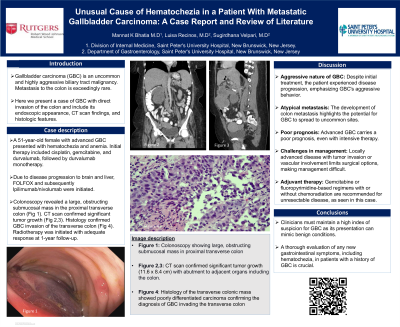
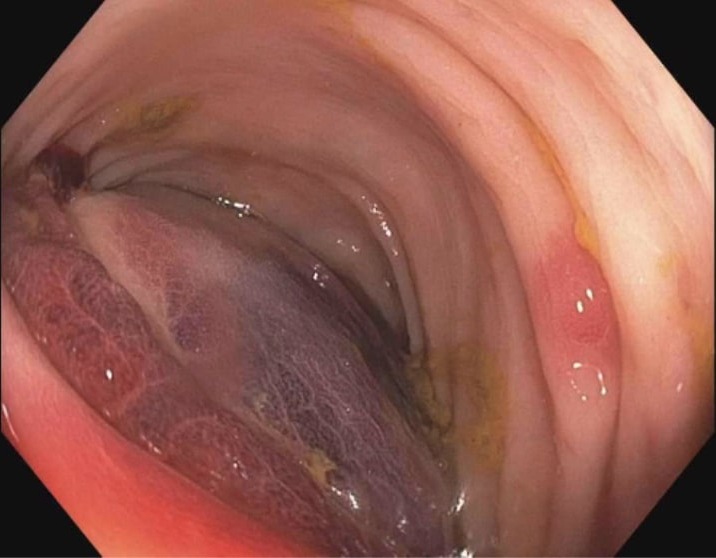
Case Description/Methods: A 51-year-old female with a history of stage 3b gallbladder carcinoma (GBC) diagnosed 1 year ago, presented with hematochezia and anemia. She had initially been treated with cisplatin, gemcitabine, and durvalumab followed by durvalumab monotherapy. Her course was complicated by brain metastasis and treatment was changed to FOLFOX therapy. Due to progression of her disease with invasion to the liver Ipilimumab/nivolumab therapy was initiated a month before presentation. On presentation, colonoscopy revealed a large, obstructing submucosal mass in the proximal transverse colon with diffuse submucosal hematoma and localized ulceration (Image 1). A CT scan of the abdomen demonstrated significant tumor growth (11.6 x 8.4 cm) with an abutment to adjacent organs including the colon. Histology of the transverse colonic mass showed poorly differentiated carcinoma confirming the diagnosis of GBC invading the transverse colon. Radiotherapy initiated for metastatic disease achieved an adequate response at one-year follow-up
Discussion: This case underscores the aggressive nature of GBC, its potential for atypical metastasis, and the poor prognosis associated with advanced stages. Management is challenging, often requiring aggressive adjuvant therapy due to limited surgical options. For patients with unresectable disease, adjuvant therapy with gemcitabine or fluoropyrimidine-based regimens with or without chemoradiation is recommended, which is reflected in the aggressive treatment approach used in this case. Despite intensive treatment, survival rates remain low. Given GBC's propensity to mimic benign conditions, clinicians must maintain a high index of suspicion. Comprehensive evaluation of any new gastrointestinal symptoms, including hematochezia, is imperative in patients with a history of GBC.
Disclosures:
Mannat Kaur. Bhatia, MD, Luisa Recinos, MD, Sugirdhana Velpari, MD. P0172 - Unusual Cause of Hematochezia in a Patient With Metastatic Gallbladder Carcinoma: A Case Report and Review of Literature, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ
Introduction: Gallbladder carcinoma (GBC) is a rare and aggressive biliary tract malignancy often mimicking benign disease, leading to delayed diagnosis and poor prognosis. The reported 5-year survival rates are 80% (stage 0), 50% (stage I), 28% (stage II), and < 10% (stages III-IV). While most GBC cases are discovered incidentally and metastasis can occur through direct invasion, peritoneal dissemination, or hematogenous dissemination, metastasis to the colon is exceedingly rare. This report presents a unique case of GBC with direct invasion into the colon, detailing endoscopic, computed tomography (CT), and histopathological findings.
Case Description/Methods: A 51-year-old female with a history of stage 3b gallbladder carcinoma (GBC) diagnosed 1 year ago, presented with hematochezia and anemia. She had initially been treated with cisplatin, gemcitabine, and durvalumab followed by durvalumab monotherapy. Her course was complicated by brain metastasis and treatment was changed to FOLFOX therapy. Due to progression of her disease with invasion to the liver Ipilimumab/nivolumab therapy was initiated a month before presentation. On presentation, colonoscopy revealed a large, obstructing submucosal mass in the proximal transverse colon with diffuse submucosal hematoma and localized ulceration (Image 1). A CT scan of the abdomen demonstrated significant tumor growth (11.6 x 8.4 cm) with an abutment to adjacent organs including the colon. Histology of the transverse colonic mass showed poorly differentiated carcinoma confirming the diagnosis of GBC invading the transverse colon. Radiotherapy initiated for metastatic disease achieved an adequate response at one-year follow-up
Discussion: This case underscores the aggressive nature of GBC, its potential for atypical metastasis, and the poor prognosis associated with advanced stages. Management is challenging, often requiring aggressive adjuvant therapy due to limited surgical options. For patients with unresectable disease, adjuvant therapy with gemcitabine or fluoropyrimidine-based regimens with or without chemoradiation is recommended, which is reflected in the aggressive treatment approach used in this case. Despite intensive treatment, survival rates remain low. Given GBC's propensity to mimic benign conditions, clinicians must maintain a high index of suspicion. Comprehensive evaluation of any new gastrointestinal symptoms, including hematochezia, is imperative in patients with a history of GBC.
Figure: Colonoscopy image showing large, obstructing submucosal mass in the proximal transverse colon with diffuse submucosal hematoma and localized ulceration.
Disclosures:
Mannat Bhatia indicated no relevant financial relationships.
Luisa Recinos indicated no relevant financial relationships.
Sugirdhana Velpari indicated no relevant financial relationships.
Mannat Kaur. Bhatia, MD, Luisa Recinos, MD, Sugirdhana Velpari, MD. P0172 - Unusual Cause of Hematochezia in a Patient With Metastatic Gallbladder Carcinoma: A Case Report and Review of Literature, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
