Sunday Poster Session
Category: Biliary/Pancreas
P0179 - Cyst Gastrostomy for a Suspected Ruptured IPMN Causing Obstructive Nephropathy
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

David Kadosh, MD
Mather Hospital, Northwell Health
Port Jefferson, NY
Presenting Author(s)
David Kadosh, MD1, Manu Dwivedi, MD1, Nathan Shamuilov, 2, Andrej Sodoma, DO3, Nick Bulba, 4, Jaspreet Singh, MD3
1Mather Hospital, Northwell Health, Port Jefferson, NY; 2New York Institute of Technology College of Osteopathic Medicine, Fresh Meadows, NY; 3Northwell Health, Bayshore, NY; 4New York Institute of Technology College of Osteopathic Medicine, Bayshore, NY
Introduction: Pancreatic pseudocysts are well circumscribed collections developing weeks after an episode of pancreatitis. Rarely, a pancreatic collection can rapidly develop in the setting of enlarging intraductal papillary mucinous neoplasms (IPMN) that rupture. In our case we describe a ruptured IPMN causing ureteral obstruction successfully managed with endoscopic cystgastrostomy.
Case Description/Methods: 95-year-old Female with a history of heart failure, sick sinus syndrome, atrial fibrillation, and DVT on Pradaxa presented to the ER with 1 week of abdominal pain radiating to the back. CT imaging was significant for mild intrahepatic biliary dilation, severe pancreatic ductal dilation with atrophy of the pancreatic parenchyma, new pancreatic cyst collection measuring 11x7 cm with compression of adjacent ureter causing hydronephrosis. Laboratory values were significant for a white blood cell count of 15k, hemoglobin of 11.8 and lipase 8. After a multi-disciplinary review a EUS guided cystgastrostomy via 15mm hot axios (LAMS) was performed. 200cc of yellow tinged fluid was drained and repeated CT imaging showed interval decrease in size of collection to 3.1x1.2 cm as well as resolution of hydronephrosis. Aspiration cytology was negative for malignant cells and showed acute/chronic inflammation. Her CEA and CA-19 levels were normal. The cyst was suspected to be a main duct IPMN that ruptured. An ERCP was performed 7 days later during which the stent was removed, and the cystic space showed no retained necrotic tissue. She tolerated a regular diet and was discharged home declining further evaluation.
Discussion: Pancreatic pseudocysts form in association with acute/chronic pancreatitis, trauma, ductal obstruction and can occasionally cause mass effect on adjacent organs. It is important to distinguish between different kinds of pancreatic fluid collections since IPMNs may appear grossly similar to pancreatic pseudocysts. Treatment of pancreatic pseudocysts involves drainage via various methods. Percutaneous drainage comes with a low rate of resolution, increased infection risk, and possible fistula formations. Surgical drainage or resection is associated with high success rates though has added mortality and complication risk. Endoscopic drainage, with methods like lumen opposing stenting, has similarly high success rates as surgical drainage with lower risk of complications. Other pancreatic cysts need to be effectively classified so they can be treated accordingly based on their risk factor.

Disclosures:
David Kadosh, MD1, Manu Dwivedi, MD1, Nathan Shamuilov, 2, Andrej Sodoma, DO3, Nick Bulba, 4, Jaspreet Singh, MD3. P0179 - Cyst Gastrostomy for a Suspected Ruptured IPMN Causing Obstructive Nephropathy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mather Hospital, Northwell Health, Port Jefferson, NY; 2New York Institute of Technology College of Osteopathic Medicine, Fresh Meadows, NY; 3Northwell Health, Bayshore, NY; 4New York Institute of Technology College of Osteopathic Medicine, Bayshore, NY
Introduction: Pancreatic pseudocysts are well circumscribed collections developing weeks after an episode of pancreatitis. Rarely, a pancreatic collection can rapidly develop in the setting of enlarging intraductal papillary mucinous neoplasms (IPMN) that rupture. In our case we describe a ruptured IPMN causing ureteral obstruction successfully managed with endoscopic cystgastrostomy.
Case Description/Methods: 95-year-old Female with a history of heart failure, sick sinus syndrome, atrial fibrillation, and DVT on Pradaxa presented to the ER with 1 week of abdominal pain radiating to the back. CT imaging was significant for mild intrahepatic biliary dilation, severe pancreatic ductal dilation with atrophy of the pancreatic parenchyma, new pancreatic cyst collection measuring 11x7 cm with compression of adjacent ureter causing hydronephrosis. Laboratory values were significant for a white blood cell count of 15k, hemoglobin of 11.8 and lipase 8. After a multi-disciplinary review a EUS guided cystgastrostomy via 15mm hot axios (LAMS) was performed. 200cc of yellow tinged fluid was drained and repeated CT imaging showed interval decrease in size of collection to 3.1x1.2 cm as well as resolution of hydronephrosis. Aspiration cytology was negative for malignant cells and showed acute/chronic inflammation. Her CEA and CA-19 levels were normal. The cyst was suspected to be a main duct IPMN that ruptured. An ERCP was performed 7 days later during which the stent was removed, and the cystic space showed no retained necrotic tissue. She tolerated a regular diet and was discharged home declining further evaluation.
Discussion: Pancreatic pseudocysts form in association with acute/chronic pancreatitis, trauma, ductal obstruction and can occasionally cause mass effect on adjacent organs. It is important to distinguish between different kinds of pancreatic fluid collections since IPMNs may appear grossly similar to pancreatic pseudocysts. Treatment of pancreatic pseudocysts involves drainage via various methods. Percutaneous drainage comes with a low rate of resolution, increased infection risk, and possible fistula formations. Surgical drainage or resection is associated with high success rates though has added mortality and complication risk. Endoscopic drainage, with methods like lumen opposing stenting, has similarly high success rates as surgical drainage with lower risk of complications. Other pancreatic cysts need to be effectively classified so they can be treated accordingly based on their risk factor.

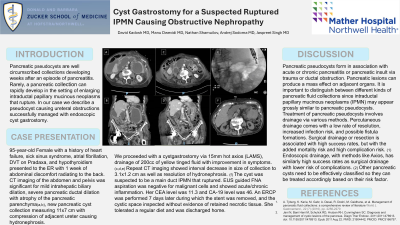
Figure: [A] Axial view of CT abd/plv notable for severely dilated pancreatic duct and large pancreatic cyst with ureteral compression
[B] Coronal view of CT abd/plv notable for severely dilated pancreatic duct and large pancreatic cyst with ureteral compression
[C] Axial view of CT abd/plv notable for lumen opposing metal stent in the decompressed cystic space
[D] Coronal view of CT abd/plv notable for lumen opposing metal stent in the decompressed cystic space
[E] Fluoroscopic imaging of lumen opposing metal stent after deployment
[F] Follow up CT imaging with improvement in pancreatic dilation and no cystic collection noted
[B] Coronal view of CT abd/plv notable for severely dilated pancreatic duct and large pancreatic cyst with ureteral compression
[C] Axial view of CT abd/plv notable for lumen opposing metal stent in the decompressed cystic space
[D] Coronal view of CT abd/plv notable for lumen opposing metal stent in the decompressed cystic space
[E] Fluoroscopic imaging of lumen opposing metal stent after deployment
[F] Follow up CT imaging with improvement in pancreatic dilation and no cystic collection noted
Disclosures:
David Kadosh indicated no relevant financial relationships.
Manu Dwivedi indicated no relevant financial relationships.
Nathan Shamuilov indicated no relevant financial relationships.
Andrej Sodoma indicated no relevant financial relationships.
Nick Bulba indicated no relevant financial relationships.
Jaspreet Singh indicated no relevant financial relationships.
David Kadosh, MD1, Manu Dwivedi, MD1, Nathan Shamuilov, 2, Andrej Sodoma, DO3, Nick Bulba, 4, Jaspreet Singh, MD3. P0179 - Cyst Gastrostomy for a Suspected Ruptured IPMN Causing Obstructive Nephropathy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
