Sunday Poster Session
Category: Biliary/Pancreas
P0180 - A Rare Presentation of Fistulizing Necrotizing Pancreatitis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- JD
Jessica Demes, MD
Brooke Army Medical Center
Fort Sam Houston, TX
Presenting Author(s)
Jessica Demes, MD, Seth Dukes, MD
Brooke Army Medical Center, Fort Sam Houston, TX
Introduction: Gastrointestinal fistulization is a rare and challenging delayed complication of necrotizing pancreatitis. Fistulization occurs in 8% of necrotizing pancreatitis patients and is associated with poorer clinical outcomes. Location of fistula may involve the stomach, small intestine, and colon either separately or simultaneously. Step up approach to therapy for this complication could help patients to avoid surgery. We present a case of simultaneous fistulization of necrotizing pancreatitis into the gastric fundus and descending colon.
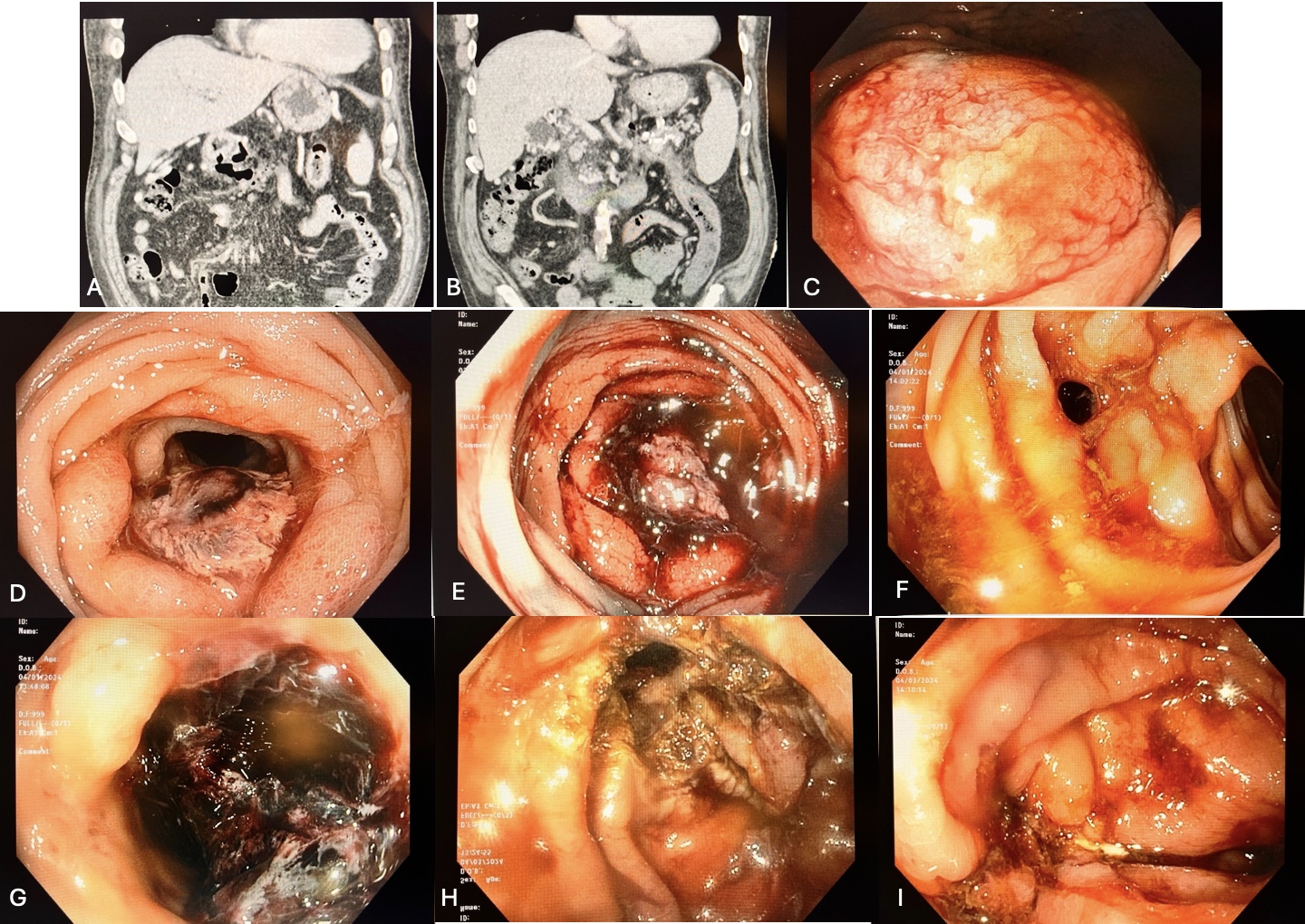
Case Description/Methods: A 60 year old male with multiple prior hospitalizations for acute on chronic pancreatitis secondary to alcohol use with multiple prior endoscopic interventions for peri-pancreatic fluid collections and pancreatic duct stricture with previously noted fistulization between pancreatic cyst cavity and duodenum and most recently development of necrotizing pancreatitis presented to the hospital with sepsis thought secondary to peri-pancreatic fluid collection. Cyst initially not amenable to drainage due to its small size and its position adjacent to the splenic artery. Patient subsequently presented 1 week later for sepsis and gastrointestinal bleeding with hematemesis and hematochezia. Bidirectional endoscopy revealed oozing gastric fundus mass and bleeding descending colon mass which required hemospray after obtaining biopsies. Computed tomography then showed concern for peripancreatic fluid collection eroding into the gastric fundus and descending colon. Patient had recurrent hematochezia with repeat colonoscopy showing blood clot present in a fistulous tract in the descending colon. Given apparent splenic artery pseudoaneurysm confluent with fistulous tract on imaging, no endoscopic intervention was attempted at that time. Interventional radiology embolized splenic artery pseudoaneurysm. Flexible sigmoidoscopy was then performed with argon plasma coagulation to de-epithealize the fistula os and endoscopic suturing device to close the fistula.
Discussion: This case demonstrates a rare and challenging to manage complication of necrotizing pancreatitis. This patient had simultaneous fistulization of peripancreatic fluid collection into the gastric fundus and colon discovered in the setting of acute gastrointestinal bleed found to be secondary to splenic artery pseudoaneurysm confluent with the fistulous tract. This case highlights the endoscopic therapeutic options available to treat this uncommon complication and help patients to avoid surgery.
Disclosures:
Jessica Demes, MD, Seth Dukes, MD. P0180 - A Rare Presentation of Fistulizing Necrotizing Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Brooke Army Medical Center, Fort Sam Houston, TX
Introduction: Gastrointestinal fistulization is a rare and challenging delayed complication of necrotizing pancreatitis. Fistulization occurs in 8% of necrotizing pancreatitis patients and is associated with poorer clinical outcomes. Location of fistula may involve the stomach, small intestine, and colon either separately or simultaneously. Step up approach to therapy for this complication could help patients to avoid surgery. We present a case of simultaneous fistulization of necrotizing pancreatitis into the gastric fundus and descending colon.
Case Description/Methods: A 60 year old male with multiple prior hospitalizations for acute on chronic pancreatitis secondary to alcohol use with multiple prior endoscopic interventions for peri-pancreatic fluid collections and pancreatic duct stricture with previously noted fistulization between pancreatic cyst cavity and duodenum and most recently development of necrotizing pancreatitis presented to the hospital with sepsis thought secondary to peri-pancreatic fluid collection. Cyst initially not amenable to drainage due to its small size and its position adjacent to the splenic artery. Patient subsequently presented 1 week later for sepsis and gastrointestinal bleeding with hematemesis and hematochezia. Bidirectional endoscopy revealed oozing gastric fundus mass and bleeding descending colon mass which required hemospray after obtaining biopsies. Computed tomography then showed concern for peripancreatic fluid collection eroding into the gastric fundus and descending colon. Patient had recurrent hematochezia with repeat colonoscopy showing blood clot present in a fistulous tract in the descending colon. Given apparent splenic artery pseudoaneurysm confluent with fistulous tract on imaging, no endoscopic intervention was attempted at that time. Interventional radiology embolized splenic artery pseudoaneurysm. Flexible sigmoidoscopy was then performed with argon plasma coagulation to de-epithealize the fistula os and endoscopic suturing device to close the fistula.
Discussion: This case demonstrates a rare and challenging to manage complication of necrotizing pancreatitis. This patient had simultaneous fistulization of peripancreatic fluid collection into the gastric fundus and colon discovered in the setting of acute gastrointestinal bleed found to be secondary to splenic artery pseudoaneurysm confluent with the fistulous tract. This case highlights the endoscopic therapeutic options available to treat this uncommon complication and help patients to avoid surgery.
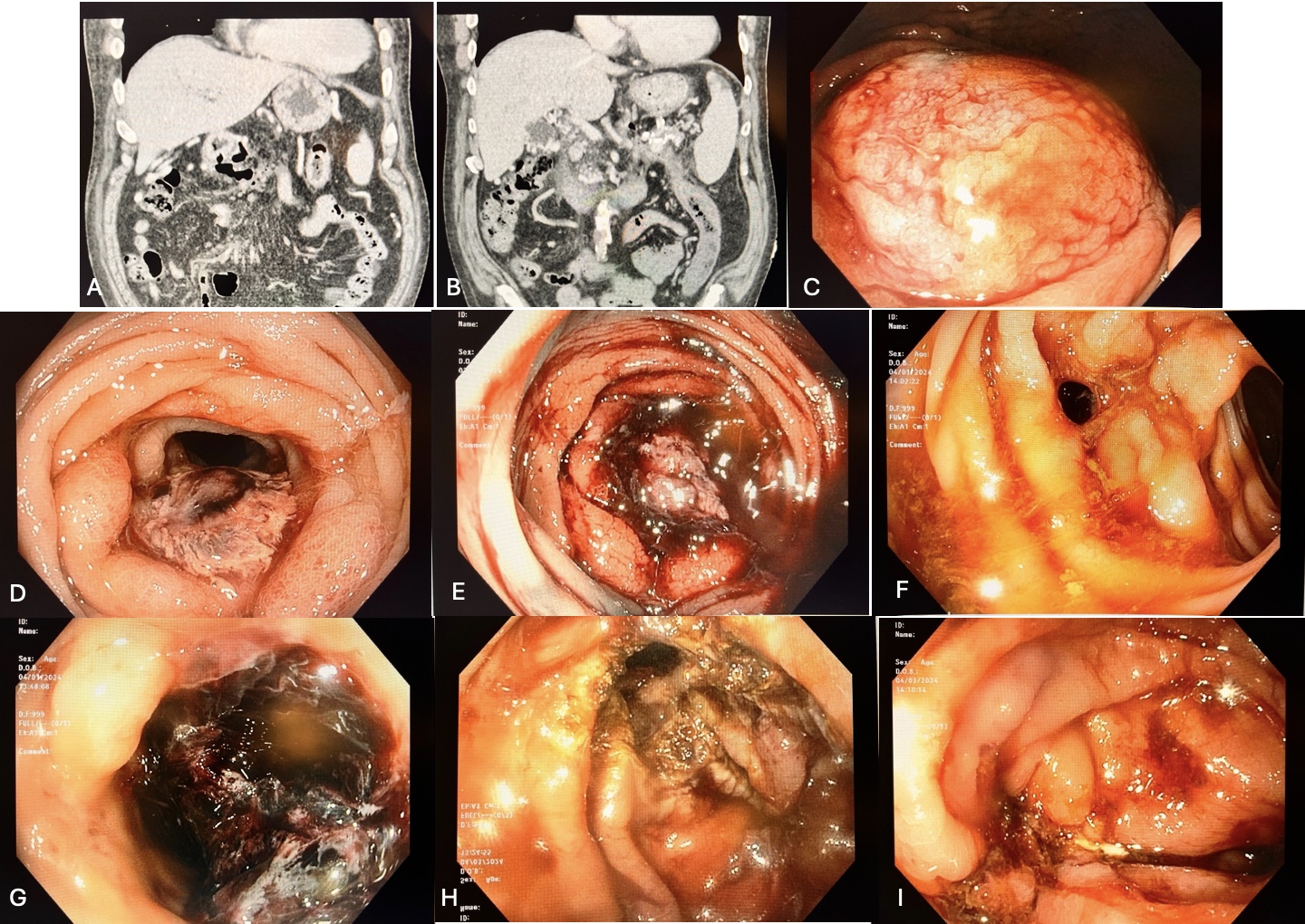
Figure: A. Computed tomography finding of necrotizing pancreatitis and peripancreatic fluid collection with fistulous tract extending to the gastric antrum; B. Computed tomography finding of peripancreatic fluid collection with fistulous tract extending to the splenic flexure; C. Upper endoscopy finding of oozing primarily subepithelial mass in the gastric fundus; D. Colonoscopy finding of 3-5cm ulcerated mass in the descending colon; E. Colonoscopy finding of bleeding descending colon mass after diagnostic biopsies; F. Subsequent colonoscopy finding of fistulous tract in the descending colon; G. Subsequent colonoscopy finding of blood clot within fistulous tract in the descending colon; H. Flexible sigmoidoscopy with descending colon fistula os de-epithelialized with argon plasma coagulation; I. Flexible sigmoidoscopy with descending colon fistula status post closure via endoscopic suturing
Disclosures:
Jessica Demes indicated no relevant financial relationships.
Seth Dukes indicated no relevant financial relationships.
Jessica Demes, MD, Seth Dukes, MD. P0180 - A Rare Presentation of Fistulizing Necrotizing Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
