Sunday Poster Session
Category: Colon
P0242 - Risk of Bleeding After Colorectal Endoscopic Mucosal Resection in Patients With Chronic Kidney Disease: A Propensity-Matched Analysis of the US Collaborative Network
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Khaled Elfert, MD
West Virginia University
Morgantown, WV
Presenting Author(s)
Khaled Elfert, MD1, Azizullah Beran, MD2, Hazem Abosheaishaa, MD3, Mouhand F.H. Mohamed, MD, MSc4, Mahmoud Nassar, MD, PhD, MSc, MPA5, Shyam Thakkar, MD1, Douglas Rex, MD2, Indira Bhavsar-Burke, MD, MHPE6, John Guardiola, MD2
1West Virginia University, Morgantown, WV; 2Indiana University School of Medicine, Indianapolis, IN; 3Icahn School of Medicine at Mount Sinai, Queens, NY; 4Mayo Clinic, Rochester, MN; 5Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, Buffalo, NY; 6University of Texas Southwestern Medical Center, Dallas, TX
Introduction: Endoscopic mucosal resection (EMR) is the most common method for resecting large ( > 20 mm) non-pedunculated colon polyps and is also used for some lesions 10-19 mm. Patients with advanced- and/or end-stage renal disease tend to have a higher risk of bleeding, the safety of EMR in advanced chronic kidney disease (CKD) patients remains under-studied. This study aimed to assess the possible adverse events associated with EMR for colorectal lesions in patients with CKD.
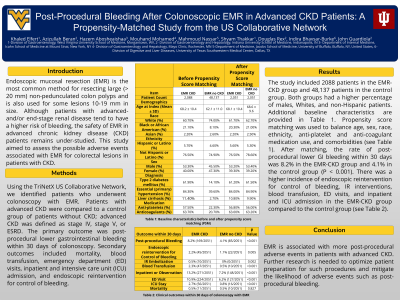
Methods: Using the TriNetX US Collaborative Network, we identified patients who underwent colonoscopy with EMR. Patients with advanced CKD were compared to a control group of patients without CKD; advanced CKD was defined as stage IV, stage V, or ESRD. The primary outcome was post-procedural lower gastrointestinal bleeding within 30 days of colonoscopy. Secondary outcomes included mortality, blood transfusion, emergency department (ED) visits, inpatient and intensive care unit (ICU) admission, and endoscopic reintervention for control of bleeding.
Results: The study included 2088 patients in the EMR-CKD group and 48,137 patients in the control group. Propensity score matching was used to balance age, sex, race, ethnicity, anti-platelet and anti-coagulant medication use, and comorbidities such as diabetes, hypertension, and cirrhosis (Table 1). After matching, the rate of post-procedural lower GI bleeding within 30 days was 8.2% in the EMR-CKD group and 4.1% in the control group (P < 0.001). There was a higher incidence of endoscopic reintervention for control of bleeding, IR interventions, blood transfusion, ED visits, and inpatient and ICU admission in the EMR-CKD group compared to the control group (Table 1).
Discussion: EMR is associated with more post-procedural adverse events in patients with advanced CKD with no difference in mortality. Further research is needed to optimize patient preparation for such procedures and mitigate the likelihood of adverse events such as post-procedural bleeding.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Khaled Elfert, MD1, Azizullah Beran, MD2, Hazem Abosheaishaa, MD3, Mouhand F.H. Mohamed, MD, MSc4, Mahmoud Nassar, MD, PhD, MSc, MPA5, Shyam Thakkar, MD1, Douglas Rex, MD2, Indira Bhavsar-Burke, MD, MHPE6, John Guardiola, MD2. P0242 - Risk of Bleeding After Colorectal Endoscopic Mucosal Resection in Patients With Chronic Kidney Disease: A Propensity-Matched Analysis of the US Collaborative Network, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1West Virginia University, Morgantown, WV; 2Indiana University School of Medicine, Indianapolis, IN; 3Icahn School of Medicine at Mount Sinai, Queens, NY; 4Mayo Clinic, Rochester, MN; 5Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, Buffalo, NY; 6University of Texas Southwestern Medical Center, Dallas, TX
Introduction: Endoscopic mucosal resection (EMR) is the most common method for resecting large ( > 20 mm) non-pedunculated colon polyps and is also used for some lesions 10-19 mm. Patients with advanced- and/or end-stage renal disease tend to have a higher risk of bleeding, the safety of EMR in advanced chronic kidney disease (CKD) patients remains under-studied. This study aimed to assess the possible adverse events associated with EMR for colorectal lesions in patients with CKD.
Methods: Using the TriNetX US Collaborative Network, we identified patients who underwent colonoscopy with EMR. Patients with advanced CKD were compared to a control group of patients without CKD; advanced CKD was defined as stage IV, stage V, or ESRD. The primary outcome was post-procedural lower gastrointestinal bleeding within 30 days of colonoscopy. Secondary outcomes included mortality, blood transfusion, emergency department (ED) visits, inpatient and intensive care unit (ICU) admission, and endoscopic reintervention for control of bleeding.
Results: The study included 2088 patients in the EMR-CKD group and 48,137 patients in the control group. Propensity score matching was used to balance age, sex, race, ethnicity, anti-platelet and anti-coagulant medication use, and comorbidities such as diabetes, hypertension, and cirrhosis (Table 1). After matching, the rate of post-procedural lower GI bleeding within 30 days was 8.2% in the EMR-CKD group and 4.1% in the control group (P < 0.001). There was a higher incidence of endoscopic reintervention for control of bleeding, IR interventions, blood transfusion, ED visits, and inpatient and ICU admission in the EMR-CKD group compared to the control group (Table 1).
Discussion: EMR is associated with more post-procedural adverse events in patients with advanced CKD with no difference in mortality. Further research is needed to optimize patient preparation for such procedures and mitigate the likelihood of adverse events such as post-procedural bleeding.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Khaled Elfert indicated no relevant financial relationships.
Azizullah Beran indicated no relevant financial relationships.
Hazem Abosheaishaa indicated no relevant financial relationships.
Mouhand Mohamed indicated no relevant financial relationships.
Mahmoud Nassar indicated no relevant financial relationships.
Shyam Thakkar indicated no relevant financial relationships.
Douglas Rex: Acacia Pharmaceuticals – Consultant. Boston Scientific – Consultant. Braintree Laboratories – Consultant, Grant/Research Support. Erbe USA – Grant/Research Support. Medivators – Grant/Research Support. Medtronic – Consultant. Norgine – Consultant. Olympus Corporation – Consultant, Grant/Research Support. Satisfai Health – Stock Options.
Indira Bhavsar-Burke indicated no relevant financial relationships.
John Guardiola: Boston Scientific Corporation – Travel Support. Olympus Corporation – Travel Support.
Khaled Elfert, MD1, Azizullah Beran, MD2, Hazem Abosheaishaa, MD3, Mouhand F.H. Mohamed, MD, MSc4, Mahmoud Nassar, MD, PhD, MSc, MPA5, Shyam Thakkar, MD1, Douglas Rex, MD2, Indira Bhavsar-Burke, MD, MHPE6, John Guardiola, MD2. P0242 - Risk of Bleeding After Colorectal Endoscopic Mucosal Resection in Patients With Chronic Kidney Disease: A Propensity-Matched Analysis of the US Collaborative Network, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
