Sunday Poster Session
Category: Colon
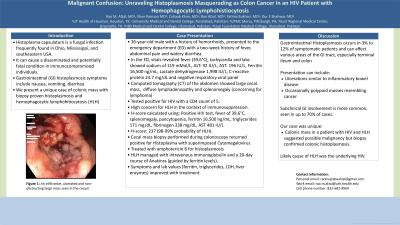
P0251 - Malignant Confusion: Unraveling Histoplasmosis Masquerading as Colon Cancer in an HIV Patient With Hemophagocytic Lymphohistiocytosis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Rao Afzal, MD
University of Pittsburgh Medical Center - Mercy
Pittsburgh, PA
Presenting Author(s)
Rao Afzal, MD1, Noor Ul Huda Ramzan, MD2, Zuhaab U. Khan, MD1, Rao Mustafa Afzal, MD3, Fatima Bukhari, MBBS4, Dur E Shahwar, MD5
1University of Pittsburgh Medical Center - Mercy, Pittsburgh, PA; 2University Medical and Dental College, Pittsburgh, PA; 3Hunt Regional Healthcare, Greenville, TX; 4Hazrat Bari Sarkar Medical and Dental College, Islamabad, Islamabad, Pakistan; 5Foundation University Medical College, Pittsburgh, PA
Introduction: Histoplasma capsulatum, a fungal infection, is frequently found in Ohio, Mississippi, and southeastern USA. In immunocompromised individuals, it causes a disseminated and potentially fatal condition. Gastrointestinal (GI) histoplasmosis symptoms include nausea, vomiting, or diarrhea. We present a unique case of colonic mass with biopsy-proven histoplasmosis complicated by hemophagocytic lymphohistiocytosis (HLH) in an HIV patient.
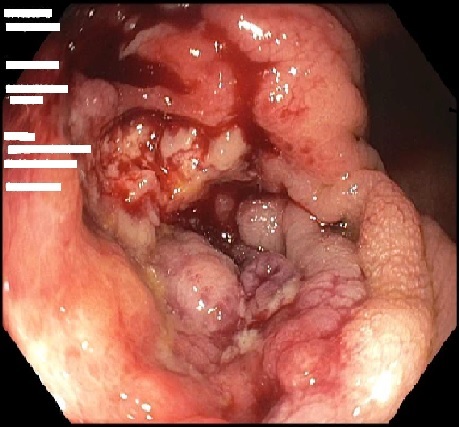
Case Description/Methods: 36 year old male with a history of hemorrhoids presented to the emergency department (ED) with a two week history of fever, abdominal pain and watery diarrhea. He denied sick contacts, recent travel outside the USA, or antibiotic use. In the ED, he had a fever of 39.6°C and tachycardia. Labs showed sodium of 119 mMol/L, ALT of 92 IU/L, and AST of 196 IU/L. Respiratory viral panel testing was negative. Computed tomography imaging of the abdomen showed a large cecal mass, diffuse lymphadenopathy and splenomegaly, concerning for lymphoma. He was tested for Human Immunodeficiency Virus (HIV), which returned positive with a CD4 count of 5. Inflammatory markers showed a ferritin level 16,500 ng/mL, lactate dehydrogenase 1,998 IU/L, and C-reactive protein 24.7 mg/dL. In the context of immunosuppression, this was concerning for hemophagocytic lymphohistiocytosis (HLH). H-score was calculated using positive HIV test, fever of 39.6°C, splenomegaly, pancytopenia, ferritin level 16,500 ng/mL, triglycerides 171 mg/dL, fibrinogen 338 mg/dL and AST 481 IU/L. He scored a 237 corresponding to a 98-99% probability of HLH. Interestingly, cecal mass biopsy obtained during colonoscopy, was positive for Histoplasma with superimposed Cytomegalovirus. He was given Amphotericin B for histoplasmosis. HLH was managed with intravenous immunoglobulin followed by a 20-day course of Anakinra guided by ferritin levels. His symptoms and labs including ferritin, triglycerides, LDH and liver enzymes, improved with treatment.
Discussion: Gastrointestinal Histoplasmosis occurs in 3% to 12% of symptomatic patients. Histoplasmosis can affect various GI tract areas, especially the terminal ileum and colon. It can present with ulcerations similar to inflammatory bowel disease and occasionally polypoid masses resembling cancer. However, subclinical GI involvement is more common, seen in up to 70% of cases. Our case was unique as colonic mass with HIV and HLH indicated possible malignancy, but biopsy confirmed colonic histoplasmosis. The likely cause of HLH was the underlying HIV.
Disclosures:
Rao Afzal, MD1, Noor Ul Huda Ramzan, MD2, Zuhaab U. Khan, MD1, Rao Mustafa Afzal, MD3, Fatima Bukhari, MBBS4, Dur E Shahwar, MD5. P0251 - Malignant Confusion: Unraveling Histoplasmosis Masquerading as Colon Cancer in an HIV Patient With Hemophagocytic Lymphohistiocytosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Pittsburgh Medical Center - Mercy, Pittsburgh, PA; 2University Medical and Dental College, Pittsburgh, PA; 3Hunt Regional Healthcare, Greenville, TX; 4Hazrat Bari Sarkar Medical and Dental College, Islamabad, Islamabad, Pakistan; 5Foundation University Medical College, Pittsburgh, PA
Introduction: Histoplasma capsulatum, a fungal infection, is frequently found in Ohio, Mississippi, and southeastern USA. In immunocompromised individuals, it causes a disseminated and potentially fatal condition. Gastrointestinal (GI) histoplasmosis symptoms include nausea, vomiting, or diarrhea. We present a unique case of colonic mass with biopsy-proven histoplasmosis complicated by hemophagocytic lymphohistiocytosis (HLH) in an HIV patient.
Case Description/Methods: 36 year old male with a history of hemorrhoids presented to the emergency department (ED) with a two week history of fever, abdominal pain and watery diarrhea. He denied sick contacts, recent travel outside the USA, or antibiotic use. In the ED, he had a fever of 39.6°C and tachycardia. Labs showed sodium of 119 mMol/L, ALT of 92 IU/L, and AST of 196 IU/L. Respiratory viral panel testing was negative. Computed tomography imaging of the abdomen showed a large cecal mass, diffuse lymphadenopathy and splenomegaly, concerning for lymphoma. He was tested for Human Immunodeficiency Virus (HIV), which returned positive with a CD4 count of 5. Inflammatory markers showed a ferritin level 16,500 ng/mL, lactate dehydrogenase 1,998 IU/L, and C-reactive protein 24.7 mg/dL. In the context of immunosuppression, this was concerning for hemophagocytic lymphohistiocytosis (HLH). H-score was calculated using positive HIV test, fever of 39.6°C, splenomegaly, pancytopenia, ferritin level 16,500 ng/mL, triglycerides 171 mg/dL, fibrinogen 338 mg/dL and AST 481 IU/L. He scored a 237 corresponding to a 98-99% probability of HLH. Interestingly, cecal mass biopsy obtained during colonoscopy, was positive for Histoplasma with superimposed Cytomegalovirus. He was given Amphotericin B for histoplasmosis. HLH was managed with intravenous immunoglobulin followed by a 20-day course of Anakinra guided by ferritin levels. His symptoms and labs including ferritin, triglycerides, LDH and liver enzymes, improved with treatment.
Discussion: Gastrointestinal Histoplasmosis occurs in 3% to 12% of symptomatic patients. Histoplasmosis can affect various GI tract areas, especially the terminal ileum and colon. It can present with ulcerations similar to inflammatory bowel disease and occasionally polypoid masses resembling cancer. However, subclinical GI involvement is more common, seen in up to 70% of cases. Our case was unique as colonic mass with HIV and HLH indicated possible malignancy, but biopsy confirmed colonic histoplasmosis. The likely cause of HLH was the underlying HIV.
Figure: An infiltrative, ulcerated and non-obstructing large mass seen in the cecum
Disclosures:
Rao Afzal indicated no relevant financial relationships.
Noor Ul Huda Ramzan indicated no relevant financial relationships.
Zuhaab Khan indicated no relevant financial relationships.
Rao Mustafa Afzal indicated no relevant financial relationships.
Fatima Bukhari indicated no relevant financial relationships.
Dur E Shahwar indicated no relevant financial relationships.
Rao Afzal, MD1, Noor Ul Huda Ramzan, MD2, Zuhaab U. Khan, MD1, Rao Mustafa Afzal, MD3, Fatima Bukhari, MBBS4, Dur E Shahwar, MD5. P0251 - Malignant Confusion: Unraveling Histoplasmosis Masquerading as Colon Cancer in an HIV Patient With Hemophagocytic Lymphohistiocytosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
