Sunday Poster Session
Category: Colon
P0287 - A Case of Ischemic Colitis Masking as Malignant Tumor
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Oladimeji E. Oluaderounmu, MD
NYC Health + Hospitals/Metropolitan
New York, NY
Presenting Author(s)
Oladimeji E. Oluaderounmu, MD1, Yamama Al-Khazraji, MD1, Bryan S. Quintanilla Rodriguez, MD2, Julio C. Valencia-Manrique, MD1, Jennifer Harley, MD1
1NYC Health + Hospitals/Metropolitan, New York, NY; 2New York Medical College - Metropolitan Hospital, New York, NY
Introduction: Ischemic colitis, a vascular condition affecting the gastrointestinal tract, results from a partial or complete occlusion of blood supply to the colon. Often underdiagnosed due to varied clinical presentations, it can sometimes mimic malignancy during imaging or endoscopic examinations.
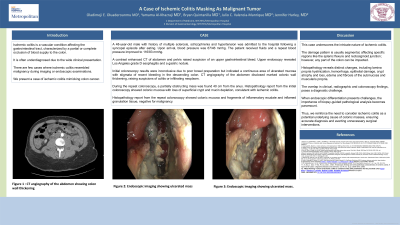
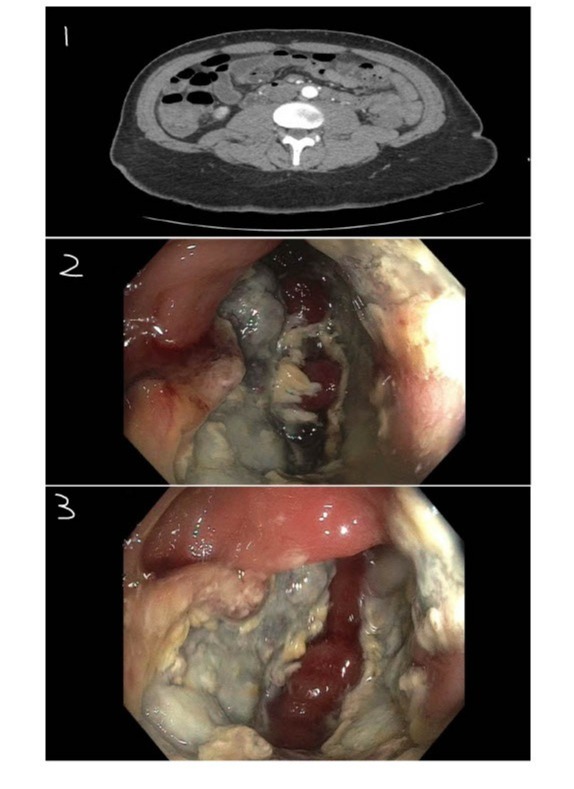
Case Description/Methods: A 48-year-old male with a history of multiple sclerosis, schizophrenia, and hypertension was admitted following a syncopal episode after eating. On arrival, his blood pressure was low at 67/46 mmHg but improved to 116/83 mmHg after fluids. A contrast-enhanced CT scan of the abdomen and pelvis suggested an upper gastrointestinal bleed. An upper endoscopy revealed Los Angeles grade D esophagitis. Initial colonoscopy was inconclusive due to poor preparation but indicated a continuous area of ulcerated mucosa with signs of recent bleeding in the descending colon. CT angiography raised suspicions of colitis or an infiltrating neoplasm due to marked colonic wall thickening (Fig 1). A repeat colonoscopy revealed a partially obstructing mass 40 cm from the anus (Fig 2, 3). Histopathology from the initial colonoscopy showed colonic mucosa with loss of superficial crypts and mucin depletion, consistent with ischemic colitis. Histopathology from the repeat colonoscopy revealed colonic mucosa and fragments of inflammatory exudate and inflamed granulation tissue, with no evidence of malignancy
Discussion: This case highlights the complex nature of ischemic colitis. Often affecting the elderly, it localizes in the left and sigmoid colon exhibiting a characteristic segmental damage (i.e. splenic flexure and rectosigmoid junction) due to changes in small blood vessels or alterations in splanchnic blood flow, though any part of the colon can be affected. Histopathological features include lamina propria hyalinization, hemorrhage, epithelial damage, crypt atrophy, and loss, along with edema and fibrosis of the submucosa and muscularis propria. The presented case involved a patient with no prior colonoscopy who exhibited a mass-forming variant of ischemic colitis, with syncope adding to the diagnostic complexity. The overlap in clinical, radiographic, and colonoscopic findings posed a significant diagnostic challenge. This case shows the importance of biopsy-guided pathological analysis in differentiating ischemic colitis from other conditions, emphasizing the need to consider ischemic colitis as a potential cause of colonic masses to ensure accurate diagnosis and avoid unnecessary surgical interventions.
Disclosures:
Oladimeji E. Oluaderounmu, MD1, Yamama Al-Khazraji, MD1, Bryan S. Quintanilla Rodriguez, MD2, Julio C. Valencia-Manrique, MD1, Jennifer Harley, MD1. P0287 - A Case of Ischemic Colitis Masking as Malignant Tumor, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1NYC Health + Hospitals/Metropolitan, New York, NY; 2New York Medical College - Metropolitan Hospital, New York, NY
Introduction: Ischemic colitis, a vascular condition affecting the gastrointestinal tract, results from a partial or complete occlusion of blood supply to the colon. Often underdiagnosed due to varied clinical presentations, it can sometimes mimic malignancy during imaging or endoscopic examinations.
Case Description/Methods: A 48-year-old male with a history of multiple sclerosis, schizophrenia, and hypertension was admitted following a syncopal episode after eating. On arrival, his blood pressure was low at 67/46 mmHg but improved to 116/83 mmHg after fluids. A contrast-enhanced CT scan of the abdomen and pelvis suggested an upper gastrointestinal bleed. An upper endoscopy revealed Los Angeles grade D esophagitis. Initial colonoscopy was inconclusive due to poor preparation but indicated a continuous area of ulcerated mucosa with signs of recent bleeding in the descending colon. CT angiography raised suspicions of colitis or an infiltrating neoplasm due to marked colonic wall thickening (Fig 1). A repeat colonoscopy revealed a partially obstructing mass 40 cm from the anus (Fig 2, 3). Histopathology from the initial colonoscopy showed colonic mucosa with loss of superficial crypts and mucin depletion, consistent with ischemic colitis. Histopathology from the repeat colonoscopy revealed colonic mucosa and fragments of inflammatory exudate and inflamed granulation tissue, with no evidence of malignancy
Discussion: This case highlights the complex nature of ischemic colitis. Often affecting the elderly, it localizes in the left and sigmoid colon exhibiting a characteristic segmental damage (i.e. splenic flexure and rectosigmoid junction) due to changes in small blood vessels or alterations in splanchnic blood flow, though any part of the colon can be affected. Histopathological features include lamina propria hyalinization, hemorrhage, epithelial damage, crypt atrophy, and loss, along with edema and fibrosis of the submucosa and muscularis propria. The presented case involved a patient with no prior colonoscopy who exhibited a mass-forming variant of ischemic colitis, with syncope adding to the diagnostic complexity. The overlap in clinical, radiographic, and colonoscopic findings posed a significant diagnostic challenge. This case shows the importance of biopsy-guided pathological analysis in differentiating ischemic colitis from other conditions, emphasizing the need to consider ischemic colitis as a potential cause of colonic masses to ensure accurate diagnosis and avoid unnecessary surgical interventions.
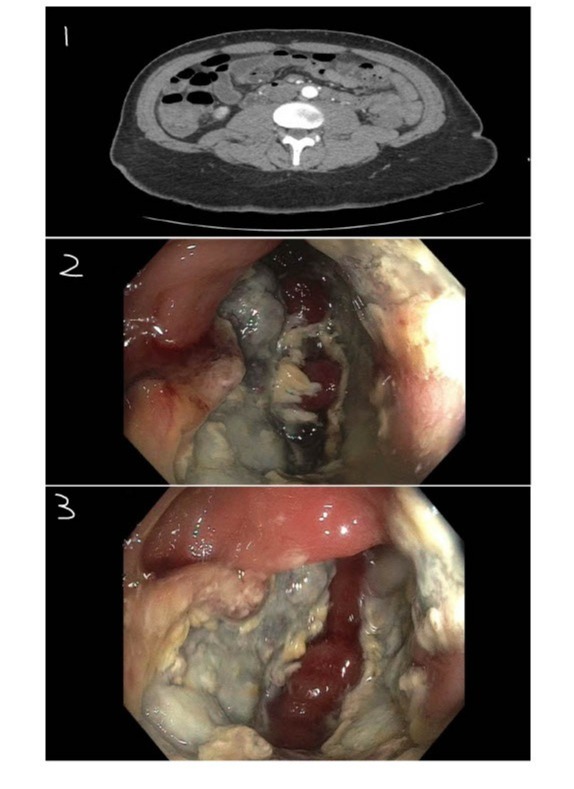
Figure: 1. CT angiography of the abdomen showing colon wall thickening
2.. Endoscopic imaging showing ulcerated mass
3. Endoscopic imaging showing ulcerated mass.
2.. Endoscopic imaging showing ulcerated mass
3. Endoscopic imaging showing ulcerated mass.
Disclosures:
Oladimeji Oluaderounmu indicated no relevant financial relationships.
Yamama Al-Khazraji indicated no relevant financial relationships.
Bryan Quintanilla Rodriguez indicated no relevant financial relationships.
Julio Valencia-Manrique indicated no relevant financial relationships.
Jennifer Harley indicated no relevant financial relationships.
Oladimeji E. Oluaderounmu, MD1, Yamama Al-Khazraji, MD1, Bryan S. Quintanilla Rodriguez, MD2, Julio C. Valencia-Manrique, MD1, Jennifer Harley, MD1. P0287 - A Case of Ischemic Colitis Masking as Malignant Tumor, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
