Sunday Poster Session
Category: Colon
P0291 - Blood and Pain: An Overlooked Diagnosis of Ischemic Colitis in Pregnancy
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Mahmoud Barbarawi, MD
DHR Health Gastroenterology
Edinburg, TX
Presenting Author(s)
Mahmoud Barbarawi, MD1, Rishika Trivedi, MD2, Majdie Salahie, MD1, Murthy Badiga, MD1, Carlos Cardenas, MD1, Asif Zamir, MD, FACG1
1DHR Health Gastroenterology, Edinburg, TX; 2DHR Health, Edinburg, TX
Introduction: Ischemic colitis, resulting from diminished blood supply to the colon, typically affects elderly patients with cardiovascular comorbidities. The mean age of presentation is 69 years, with only 2.7% of cases occurring in adults under 45. Significant large bowel ischemia is rarely seen among younger individuals, particularly pregnant women.
Case Description/Methods: A 35-year-old Hispanic woman in her eighth week of pregnancy presented with a 24-hour history of lower abdominal cramping, accompanied by 5-6 episodes of bloody diarrhea, that was preceded by nausea, and vomiting. Her medical history was unremarkable, with no recent travel, antibiotic usage, family history of inflammatory bowel disease, or coagulopathy. On admission, her BMI was 37, and her vital signs were stable. Initial lab findings showed a slightly elevated white blood cell count of 12,200 with 41.9% lymphocytes. Tests ruled out viral, bacterial, and parasitic infections.
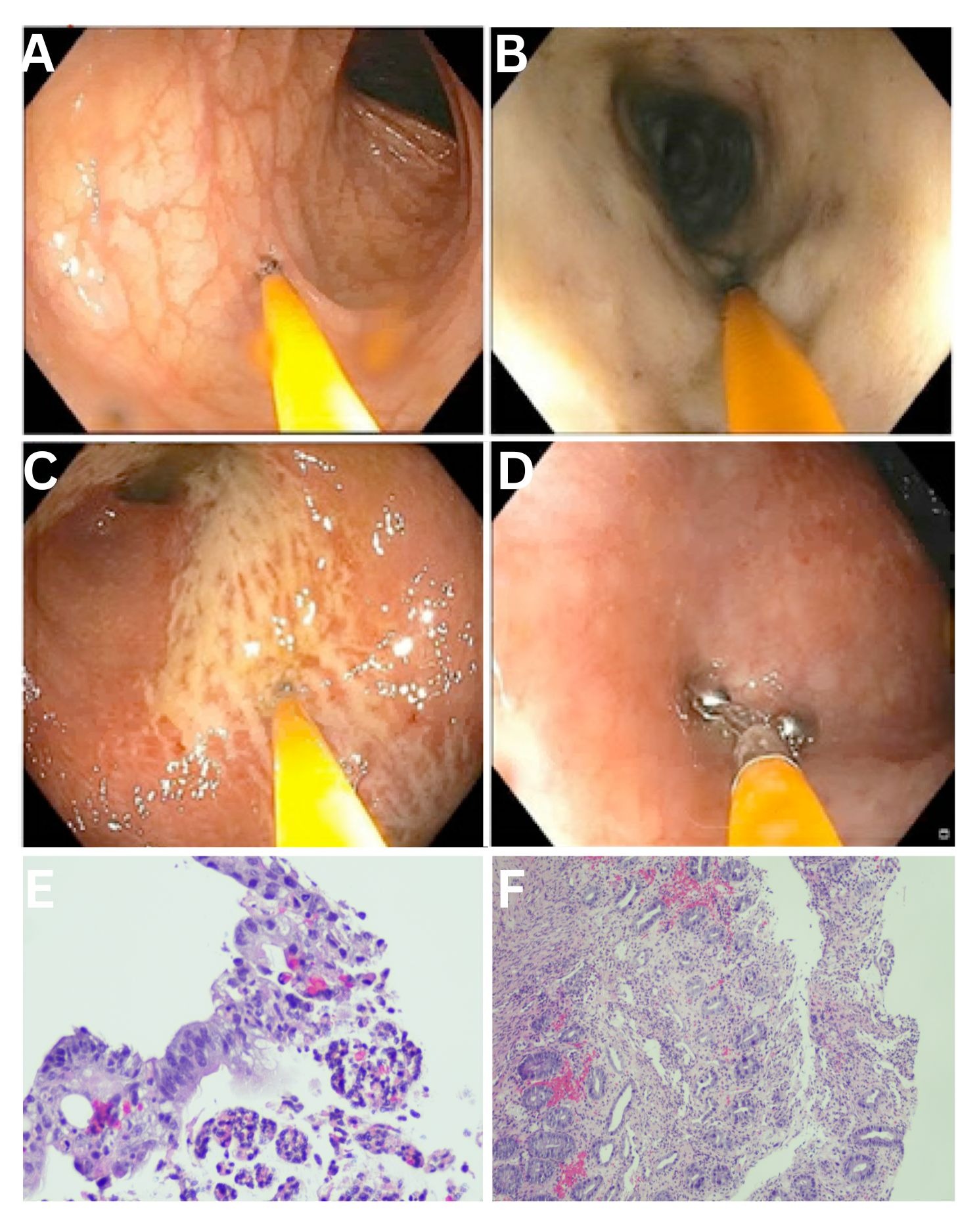
Colonoscopy revealed loss of vascular pattern, exudate, and ulcerations extending from the descending colon to the rectosigmoid. Biopsies from various colonic segments showed focal cryptitis, crypt dropout, and fibrosis, indicative of ischemic changes. Ultrasound Doppler examination revealed increased velocities within the inferior mesenteric artery, supporting the diagnosis of ischemic colitis. Tests for antithrombin 3 deficiency, protein C and S deficiency, and antiphospholipid antibody syndrome were negative.
Due to the potential risks of radiation exposure to the developing fetus, CT scans with contrast and MRI angiography were avoided. The patient was managed conservatively with intravenous fluid resuscitation and electrolyte replacement, leading to rapid and complete recovery.
Discussion: This case underscores the importance of considering ischemic colitis in the differential diagnosis of abdominal pain and bloody diarrhea, even in atypical patient populations such as young pregnant women. Our working hypothesis for this patient's development of ischemic colitis is that she experienced gastroenteritis with resultant excessive vomiting, and without proper hydration therapy, this led to intravascular volume depletion, predisposing her to ischemic colitis. This case illustrates that conservative management can be effective, ensuring both maternal and fetal safety. To prevent such cases, maintaining adequate hydration is considered key in managing patients with excessive vomiting and potential volume depletion.
Disclosures:
Mahmoud Barbarawi, MD1, Rishika Trivedi, MD2, Majdie Salahie, MD1, Murthy Badiga, MD1, Carlos Cardenas, MD1, Asif Zamir, MD, FACG1. P0291 - Blood and Pain: An Overlooked Diagnosis of Ischemic Colitis in Pregnancy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1DHR Health Gastroenterology, Edinburg, TX; 2DHR Health, Edinburg, TX
Introduction: Ischemic colitis, resulting from diminished blood supply to the colon, typically affects elderly patients with cardiovascular comorbidities. The mean age of presentation is 69 years, with only 2.7% of cases occurring in adults under 45. Significant large bowel ischemia is rarely seen among younger individuals, particularly pregnant women.
Case Description/Methods: A 35-year-old Hispanic woman in her eighth week of pregnancy presented with a 24-hour history of lower abdominal cramping, accompanied by 5-6 episodes of bloody diarrhea, that was preceded by nausea, and vomiting. Her medical history was unremarkable, with no recent travel, antibiotic usage, family history of inflammatory bowel disease, or coagulopathy. On admission, her BMI was 37, and her vital signs were stable. Initial lab findings showed a slightly elevated white blood cell count of 12,200 with 41.9% lymphocytes. Tests ruled out viral, bacterial, and parasitic infections.
Colonoscopy revealed loss of vascular pattern, exudate, and ulcerations extending from the descending colon to the rectosigmoid. Biopsies from various colonic segments showed focal cryptitis, crypt dropout, and fibrosis, indicative of ischemic changes. Ultrasound Doppler examination revealed increased velocities within the inferior mesenteric artery, supporting the diagnosis of ischemic colitis. Tests for antithrombin 3 deficiency, protein C and S deficiency, and antiphospholipid antibody syndrome were negative.
Due to the potential risks of radiation exposure to the developing fetus, CT scans with contrast and MRI angiography were avoided. The patient was managed conservatively with intravenous fluid resuscitation and electrolyte replacement, leading to rapid and complete recovery.
Discussion: This case underscores the importance of considering ischemic colitis in the differential diagnosis of abdominal pain and bloody diarrhea, even in atypical patient populations such as young pregnant women. Our working hypothesis for this patient's development of ischemic colitis is that she experienced gastroenteritis with resultant excessive vomiting, and without proper hydration therapy, this led to intravascular volume depletion, predisposing her to ischemic colitis. This case illustrates that conservative management can be effective, ensuring both maternal and fetal safety. To prevent such cases, maintaining adequate hydration is considered key in managing patients with excessive vomiting and potential volume depletion.
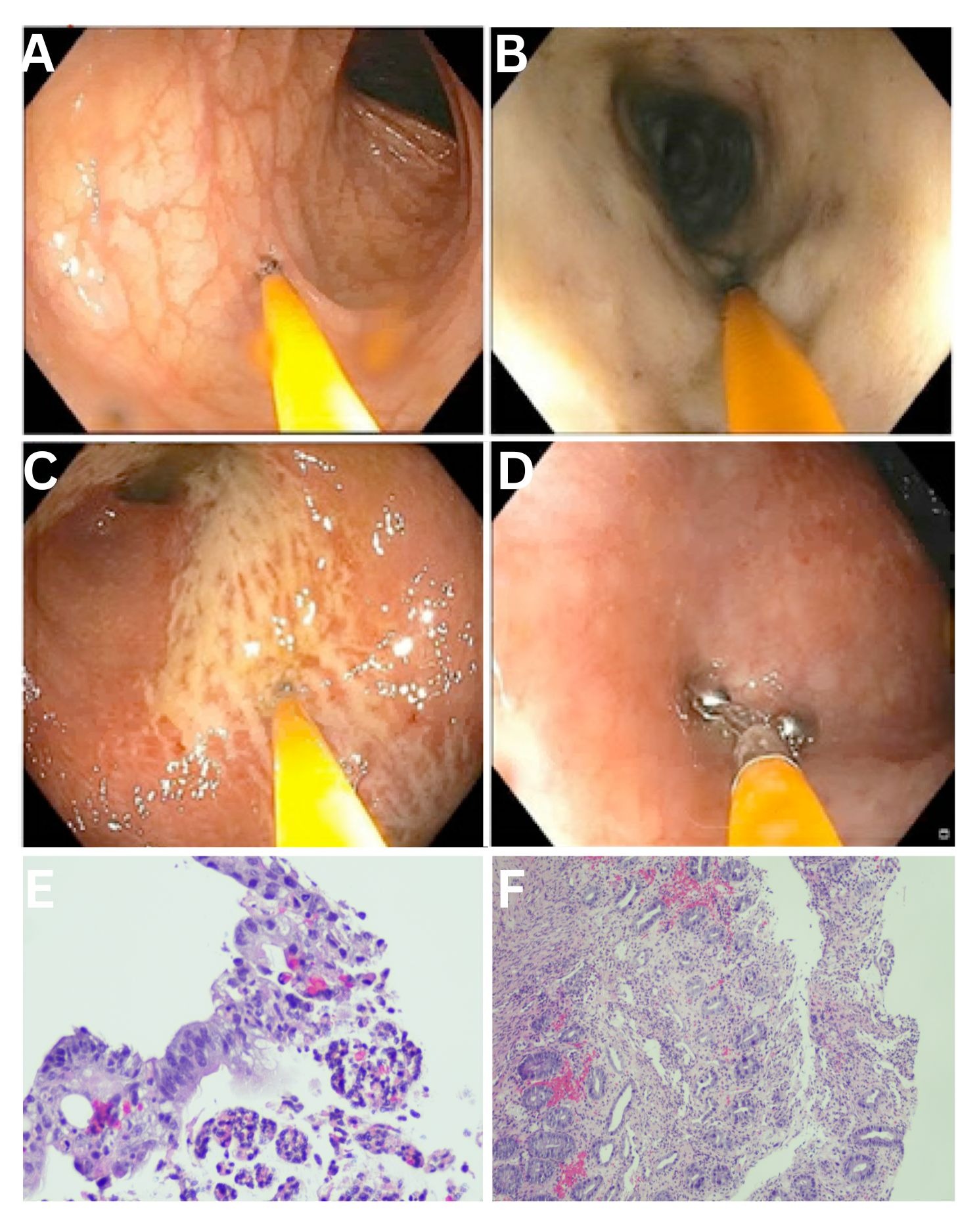
Figure: Figure A: Splenic Flexure, showing distinct loss of vascular pattern, exudate and ulcerations.
Figure B: Descending colon, showing distinct loss of vascular pattern, exudate and ulcerations.
Figure C: Rectosigmoid, showing distinct loss of vascular pattern, exudate and ulcerations.
Figure D: Rectum, showing distinct loss of vascular pattern, exudate and ulcerations.
Figure E: Histological findings from the biopsy specimen revealed fibrosis in the lamina propria along with focal cryptitis.
Figure F: Histological findings from biopsy specimen revealed crypt loss and dropout.
Figure B: Descending colon, showing distinct loss of vascular pattern, exudate and ulcerations.
Figure C: Rectosigmoid, showing distinct loss of vascular pattern, exudate and ulcerations.
Figure D: Rectum, showing distinct loss of vascular pattern, exudate and ulcerations.
Figure E: Histological findings from the biopsy specimen revealed fibrosis in the lamina propria along with focal cryptitis.
Figure F: Histological findings from biopsy specimen revealed crypt loss and dropout.
Disclosures:
Mahmoud Barbarawi indicated no relevant financial relationships.
Rishika Trivedi indicated no relevant financial relationships.
Majdie Salahie indicated no relevant financial relationships.
Murthy Badiga indicated no relevant financial relationships.
Carlos Cardenas indicated no relevant financial relationships.
Asif Zamir indicated no relevant financial relationships.
Mahmoud Barbarawi, MD1, Rishika Trivedi, MD2, Majdie Salahie, MD1, Murthy Badiga, MD1, Carlos Cardenas, MD1, Asif Zamir, MD, FACG1. P0291 - Blood and Pain: An Overlooked Diagnosis of Ischemic Colitis in Pregnancy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
