Sunday Poster Session
Category: Colon
P0297 - Symptomatic Colonic Spirochetosis in a Patient With Newly Diagnosed HIV
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Arham Siddiqui, MD
University of Texas Health San Antonio
San Antonio, TX
Presenting Author(s)
Arham Siddiqui, MD1, Parth Patel, MD1, James Gnecco, DO2, Saatchi Kuwelker, MD3, Aziz Tejani, MD1, Shane Sweeney, MD4, Chandraprakash Umapathy, MD1
1University of Texas Health San Antonio, San Antonio, TX; 2UTHSCSA, San Antonio, TX; 3University of Texas Health Science Center, San Antonio, TX; 4Audie Murphy VA Hospital, San Antonio, TX
Introduction: Colonic spirochetosis is a rare gastrointestinal pathology which is not completely understood. It can present with diarrhea, abdominal cramping, or rectal bleeding; however, it is often an incidental finding without significant clinical correlation. We present a case of symptomatic colonic spirochetosis in a patient with newly diagnosed HIV.
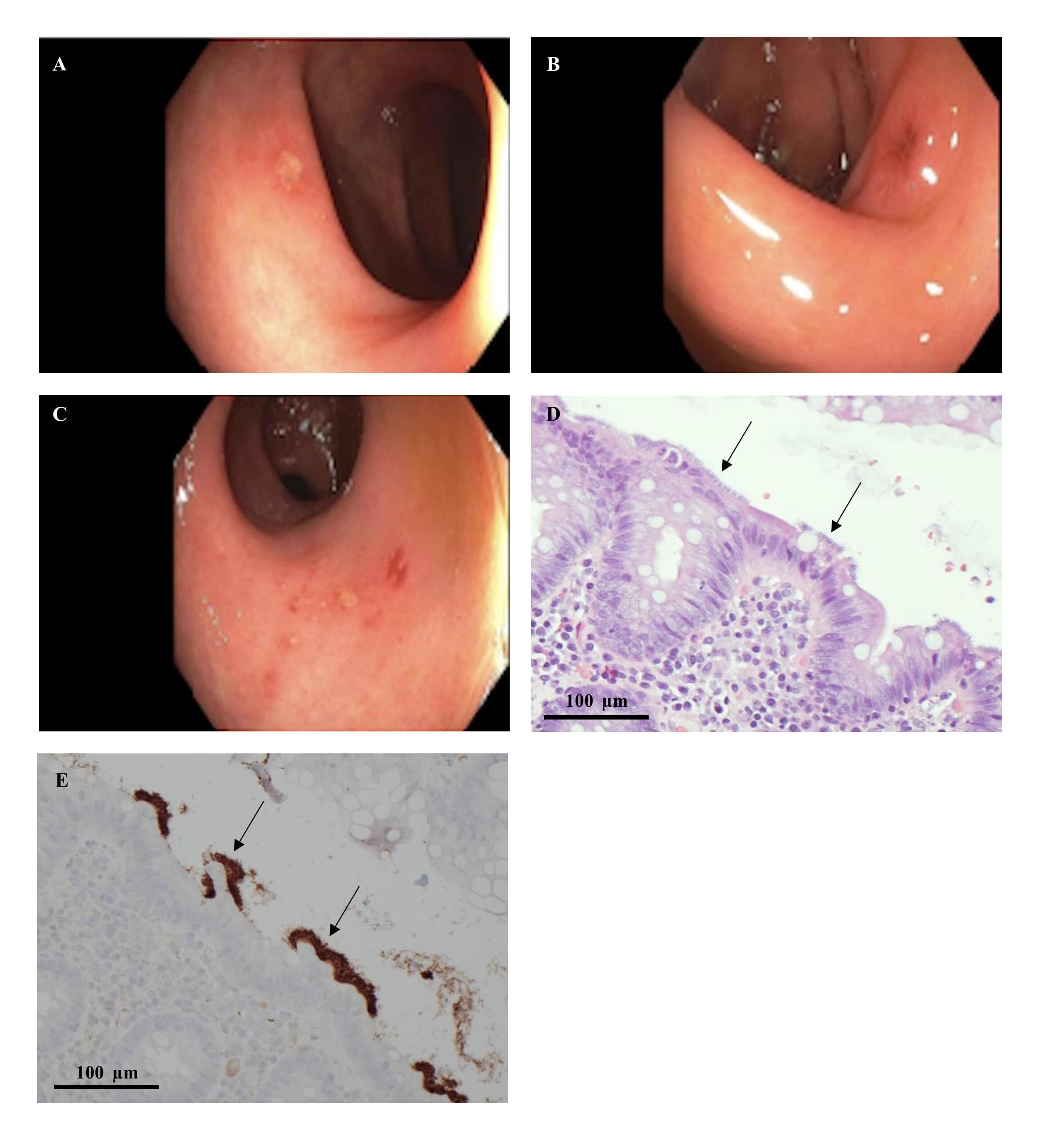
Case Description/Methods: A 53-year-old man presented for three weeks of diarrhea with no other symptoms. He has no other pertinent medical, surgical, or family history. He denied a history of sexually transmitted disease or anal intercourse. Physical exam was unremarkable. Laboratory studies showed a negative stool PCR for GI pathogens and a negative syphilis screen. CT abdomen showed mesenteric panniculitis, rectal inflammation, and perirectal lymphadenopathy. He was HIV RNA positive with a CD4 cell count of 125 cells/mm3. Flexible sigmoidoscopy revealed shallow ulcerations in the rectum and sigmoid colon with decreased vascularity (A-C). Colonic biopsies showed fragments of mucosa with a basophilic fringe on the surface epithelium (D), which is further highlighted with a spirochete immunohistochemical stain (E). He was started on Biktarvy for his HIV and his diarrhea resolved without further treatment.
Discussion: The prevalence of colonic spirochetosis (CS) is higher in developing countries; however, a risk factor in developed countries is immune status. Our patient was newly diagnosed with HIV. Opportunistic invasion of spirochetes into colonic epithelia causes mitochondrial swelling, cell membrane destruction, and decreased brush border resorption leading to diarrhea. A “false brush border” sign is pathognomonic for CS. The bacteria most commonly implicated are Brachyspira aalborgi and Brachyspira pilosicoli. The treatment of choice is metronidazole which can resolve the infection but may not always lead to symptomatic relief. The presentation of CS is non-specific and can even be subclinical. Therefore, cognizance of the disease and its management is useful once common etiologies have been ruled out. Identifying risk factors such as HIV-positive status or prior anal intercourse can cue providers into obtaining colon biopsies since histopathology will lead to definitive diagnosis.
Disclosures:
Arham Siddiqui, MD1, Parth Patel, MD1, James Gnecco, DO2, Saatchi Kuwelker, MD3, Aziz Tejani, MD1, Shane Sweeney, MD4, Chandraprakash Umapathy, MD1. P0297 - Symptomatic Colonic Spirochetosis in a Patient With Newly Diagnosed HIV, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas Health San Antonio, San Antonio, TX; 2UTHSCSA, San Antonio, TX; 3University of Texas Health Science Center, San Antonio, TX; 4Audie Murphy VA Hospital, San Antonio, TX
Introduction: Colonic spirochetosis is a rare gastrointestinal pathology which is not completely understood. It can present with diarrhea, abdominal cramping, or rectal bleeding; however, it is often an incidental finding without significant clinical correlation. We present a case of symptomatic colonic spirochetosis in a patient with newly diagnosed HIV.
Case Description/Methods: A 53-year-old man presented for three weeks of diarrhea with no other symptoms. He has no other pertinent medical, surgical, or family history. He denied a history of sexually transmitted disease or anal intercourse. Physical exam was unremarkable. Laboratory studies showed a negative stool PCR for GI pathogens and a negative syphilis screen. CT abdomen showed mesenteric panniculitis, rectal inflammation, and perirectal lymphadenopathy. He was HIV RNA positive with a CD4 cell count of 125 cells/mm3. Flexible sigmoidoscopy revealed shallow ulcerations in the rectum and sigmoid colon with decreased vascularity (A-C). Colonic biopsies showed fragments of mucosa with a basophilic fringe on the surface epithelium (D), which is further highlighted with a spirochete immunohistochemical stain (E). He was started on Biktarvy for his HIV and his diarrhea resolved without further treatment.
Discussion: The prevalence of colonic spirochetosis (CS) is higher in developing countries; however, a risk factor in developed countries is immune status. Our patient was newly diagnosed with HIV. Opportunistic invasion of spirochetes into colonic epithelia causes mitochondrial swelling, cell membrane destruction, and decreased brush border resorption leading to diarrhea. A “false brush border” sign is pathognomonic for CS. The bacteria most commonly implicated are Brachyspira aalborgi and Brachyspira pilosicoli. The treatment of choice is metronidazole which can resolve the infection but may not always lead to symptomatic relief. The presentation of CS is non-specific and can even be subclinical. Therefore, cognizance of the disease and its management is useful once common etiologies have been ruled out. Identifying risk factors such as HIV-positive status or prior anal intercourse can cue providers into obtaining colon biopsies since histopathology will lead to definitive diagnosis.
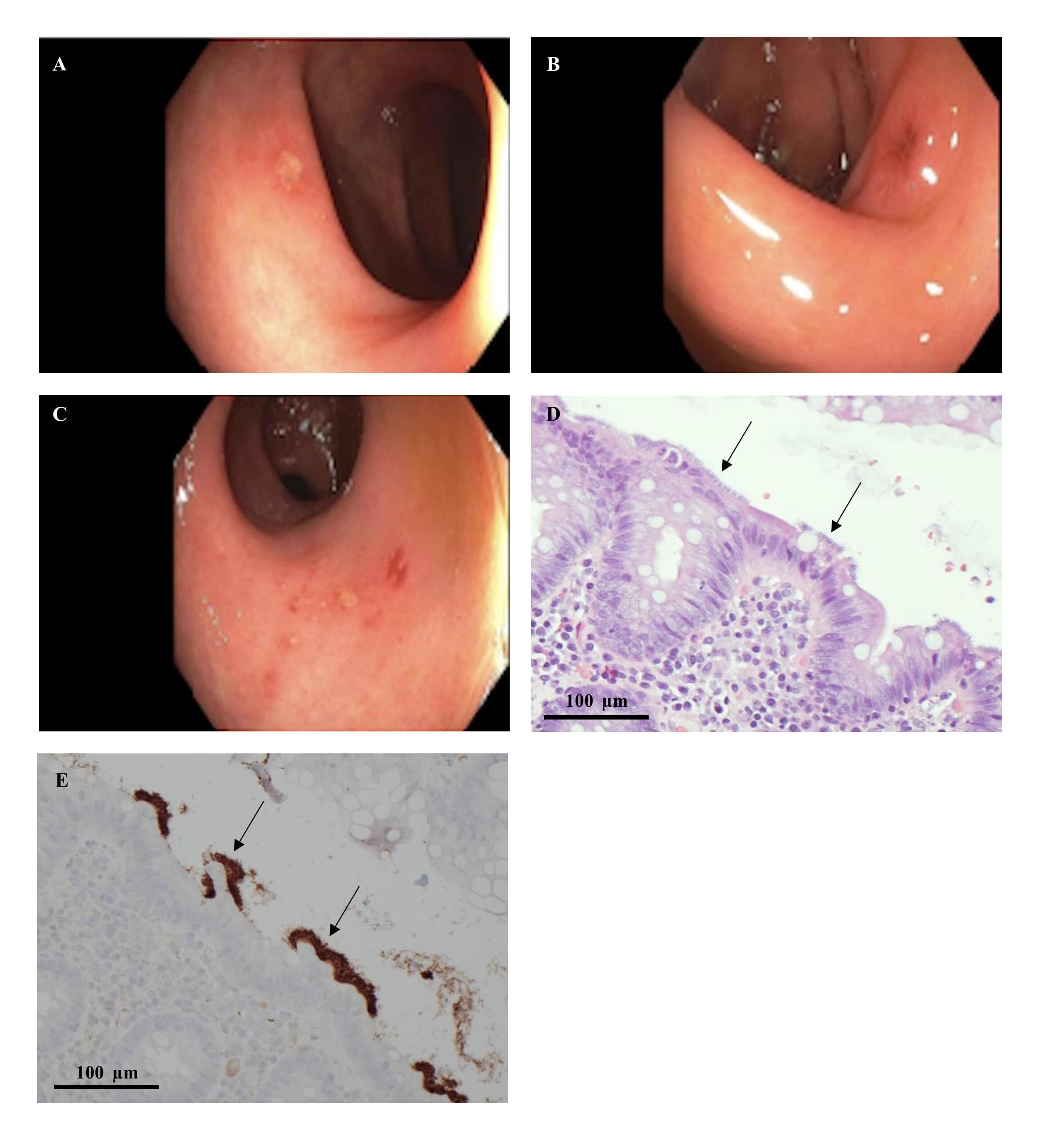
Figure: Shallow ulcerations with decreased vascularity in the sigmoid colon (A, B) and rectum (C). H&E (D) with fragments of colonic mucosa with a basophilic fringe on surface epithelium further highlighted with a spirochete immunohistochemical stain (E).
Disclosures:
Arham Siddiqui indicated no relevant financial relationships.
Parth Patel indicated no relevant financial relationships.
James Gnecco indicated no relevant financial relationships.
Saatchi Kuwelker indicated no relevant financial relationships.
Aziz Tejani indicated no relevant financial relationships.
Shane Sweeney indicated no relevant financial relationships.
Chandraprakash Umapathy indicated no relevant financial relationships.
Arham Siddiqui, MD1, Parth Patel, MD1, James Gnecco, DO2, Saatchi Kuwelker, MD3, Aziz Tejani, MD1, Shane Sweeney, MD4, Chandraprakash Umapathy, MD1. P0297 - Symptomatic Colonic Spirochetosis in a Patient With Newly Diagnosed HIV, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

