Sunday Poster Session
Category: Colon
P0321 - Stanford Type A Aortic Dissection Masquerading as Subacute Diarrhea
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Bridgette B. McNally, DO
Mayo Clinic School of Graduate Medical Education
Scottsdale, AZ
Presenting Author(s)
Bridgette B. McNally, DO1, Gassan Kassim, MD2, Allon Kahn, MD2, Dora Lam-Himlin, MD2, Suryakanth Gurudu, MD, FACG3, Alex Wallace, MD3
1Mayo Clinic School of Graduate Medical Education, Scottsdale, AZ; 2Mayo Clinic, Scottsdale, AZ; 3Mayo Clinic, Phoenix, AZ
Introduction: Intestinal ischemia is due to tissue hypoxia, varying by chronicity, location & extent of disease. Symptoms can include abdominal pain, sitophobia, diarrhea, weight loss & bleeding. We present a case of subacute mesenteric ischemia & ischemic colitis in a male presenting with 3 weeks of diarrhea, found to have an aortic dissection.
Case Description/Methods: A 60-year-old male with history of stroke, dyslipidemia & hypertension presented with 3 weeks of diarrhea after noting teeth pain & leg claudication after a workout. He had a negative cardiac work up and was given dicyclomine & antibiotics. However, due to progressive postprandial epigastric pain, watery postprandial/nocturnal diarrhea & weight loss, he presented to our facility. He denied NSAIDs or tobacco use and had no prior episodes. He had a colonoscopy 3 months prior, with a few benign polyps.
On arrival, he was hypotensive and afebrile. Labs were notable for WBC 17.3, sodium 130, potassium 3.3, bicarbonate 20, chloride 91, BUN 36, creatinine 2.3, lactate 1.9, CRP 50 & normal TSH. GI pathogen panel & C. difficile were negative. A CT abdomen and pelvis without IV contrast showed scattered fluid & air fluid levels, consistent with diarrhea. An EGD showed Forrest class III antral & incisura ulcers, congested ulcerated mucosa in the duodenum and colonoscopy showed congested ulcerated mucosa in the terminal ileum, cecum, ascending & descending colon. Histology was nonspecific, but could represent ischemia. Therefore, a mesenteric arterial doppler was obtained and showed stenosis in the celiac & superior/inferior mesenteric arteries & CT chest, abdomen and pelvis with angiography (CTA) noted Standford type A aortic dissection with abdominal pelvic extension. The patient taken for urgent aortic repair.
Discussion: Intestinal ischemia is due to altered blood flow. Chronic/subacute mesenteric ischemia occurs in < 5% of patients and is often related to atherosclerosis; 91% of cases have occlusion in at least 2 of the mesenteric vessels. It presents with postprandial abdominal pain, sitophobia, weight loss and diarrhea and CTA guides management. Colonic ischemia is related to cardiovascular risk factors, medications, vasculitis, & thrombophilic disorders. Diagnosis is made using imaging & endoscopic findings & management ranges from observation to surgery.
Our patient presented with findings of both subacute mesenteric ischemia & ischemic colitis, which led to identification of a type A aortic dissection, prompting a life-saving intervention.

Disclosures:
Bridgette B. McNally, DO1, Gassan Kassim, MD2, Allon Kahn, MD2, Dora Lam-Himlin, MD2, Suryakanth Gurudu, MD, FACG3, Alex Wallace, MD3. P0321 - Stanford Type A Aortic Dissection Masquerading as Subacute Diarrhea, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mayo Clinic School of Graduate Medical Education, Scottsdale, AZ; 2Mayo Clinic, Scottsdale, AZ; 3Mayo Clinic, Phoenix, AZ
Introduction: Intestinal ischemia is due to tissue hypoxia, varying by chronicity, location & extent of disease. Symptoms can include abdominal pain, sitophobia, diarrhea, weight loss & bleeding. We present a case of subacute mesenteric ischemia & ischemic colitis in a male presenting with 3 weeks of diarrhea, found to have an aortic dissection.
Case Description/Methods: A 60-year-old male with history of stroke, dyslipidemia & hypertension presented with 3 weeks of diarrhea after noting teeth pain & leg claudication after a workout. He had a negative cardiac work up and was given dicyclomine & antibiotics. However, due to progressive postprandial epigastric pain, watery postprandial/nocturnal diarrhea & weight loss, he presented to our facility. He denied NSAIDs or tobacco use and had no prior episodes. He had a colonoscopy 3 months prior, with a few benign polyps.
On arrival, he was hypotensive and afebrile. Labs were notable for WBC 17.3, sodium 130, potassium 3.3, bicarbonate 20, chloride 91, BUN 36, creatinine 2.3, lactate 1.9, CRP 50 & normal TSH. GI pathogen panel & C. difficile were negative. A CT abdomen and pelvis without IV contrast showed scattered fluid & air fluid levels, consistent with diarrhea. An EGD showed Forrest class III antral & incisura ulcers, congested ulcerated mucosa in the duodenum and colonoscopy showed congested ulcerated mucosa in the terminal ileum, cecum, ascending & descending colon. Histology was nonspecific, but could represent ischemia. Therefore, a mesenteric arterial doppler was obtained and showed stenosis in the celiac & superior/inferior mesenteric arteries & CT chest, abdomen and pelvis with angiography (CTA) noted Standford type A aortic dissection with abdominal pelvic extension. The patient taken for urgent aortic repair.
Discussion: Intestinal ischemia is due to altered blood flow. Chronic/subacute mesenteric ischemia occurs in < 5% of patients and is often related to atherosclerosis; 91% of cases have occlusion in at least 2 of the mesenteric vessels. It presents with postprandial abdominal pain, sitophobia, weight loss and diarrhea and CTA guides management. Colonic ischemia is related to cardiovascular risk factors, medications, vasculitis, & thrombophilic disorders. Diagnosis is made using imaging & endoscopic findings & management ranges from observation to surgery.
Our patient presented with findings of both subacute mesenteric ischemia & ischemic colitis, which led to identification of a type A aortic dissection, prompting a life-saving intervention.

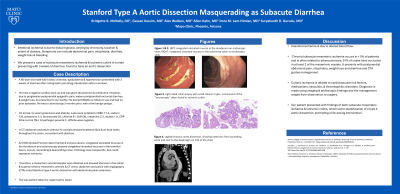
Figure: Figure 1: congested ulcerated mucosa in the duodenum on endoscopic view. Figure 2: congested ulcerated mucosa in the transverse colon on endoscopic view. Figure 3: right sided colon biopsy with small colonic crypts, reminiscent of the “microcrypts” often found in ischemic colitis. Figure 4: sagittal thoracic aorta dissection, showing extension from ascending aorta and root to the diaphragm
Disclosures:
Bridgette McNally indicated no relevant financial relationships.
Gassan Kassim indicated no relevant financial relationships.
Allon Kahn: MiMedx Inc – Consultant.
Dora Lam-Himlin indicated no relevant financial relationships.
Suryakanth Gurudu indicated no relevant financial relationships.
Alex Wallace indicated no relevant financial relationships.
Bridgette B. McNally, DO1, Gassan Kassim, MD2, Allon Kahn, MD2, Dora Lam-Himlin, MD2, Suryakanth Gurudu, MD, FACG3, Alex Wallace, MD3. P0321 - Stanford Type A Aortic Dissection Masquerading as Subacute Diarrhea, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
