Sunday Poster Session
Category: Colon
P0332 - A Chance Finding: Pneumatosis Cystoides Intestinalis in the Setting of Splenic Laceration
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- MS
Matthew Schwartz, MD
Brooke Army Medical Center
San Antonio, TX
Presenting Author(s)
Matthew Schwartz, MD, James M. Francis, DO
Brooke Army Medical Center, San Antonio, TX
Introduction: Pneumatosis cystoides intestinalis (PCI) is a rare disease characterized by the presence of gaseous cysts in the intestinal wall. We present a rare case of a PCI polyp resectioned during colonoscopy in a patient with an associated splenic laceration.
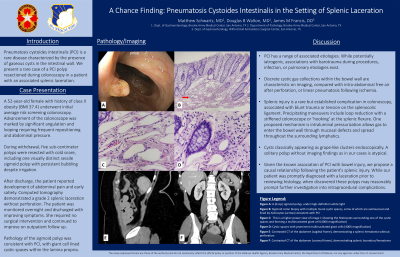
Case Description/Methods: A 52-year-old female with history of class II obesity (BMI 37.4) underwent initial average risk screening colonoscopy. Advancement of the colonoscope was marked by significant angulation and looping requiring frequent repositioning and abdominal pressure. During withdrawal, five subcentimeter polyps were resected with cold snare, including one visually distinct sessile sigmoid polyp with persistent bubbling despite irrigation. After discharge, the patient reported development of abdominal pain and early satiety. Computed tomography demonstrated a grade 2 splenic laceration without perforation. The patient was monitored overnight and discharged with improving symptoms. Pathology of the aforementioned polyp was consistent with PCI, with giant cell lined cystic spaces within the lamina propria.
Discussion: Known as pneumatosis cystoides coli when limited to the colon, PCI has a range of associated etiologies. While potentially iatrogenic, associations with barotrauma during procedures, infection, or pulmonary etiologies exist. When found on imaging, discrete cystic gas collections within the bowel wall are characteristic. This contrasts with intra-abdominal free air after perforation, or linear pneumatosis following ischemia. Cysts may also be visualized endoscopically, classically appearing as grape-like clusters.
Splenic injury is a rare but established complication in colonoscopy, associated with blunt trauma or tension on the splenocolic ligament. Precipitating maneuvers include loop reduction with a stiffened colonoscope or ‘hooking’ at the splenic flexure. In PCI seen after endoscopic or surgical interventions, it is proposed that intraluminal pressurization allows gas to enter the bowel wall through mucosal defects and spread throughout the surrounding lymphatics.
A solitary polyp in the absence of imaging findings as in our cases is atypical. Given the documented association of these polyps with bowel injury, we propose a causal relationship following the patient's splenic injury during colonoscopy. While our patient was promptly diagnosed with the laceration prior to receiving histology results, when discovered, these polyps may reasonably prompt further investigation into intraprocedural complications.

Disclosures:
Matthew Schwartz, MD, James M. Francis, DO. P0332 - A Chance Finding: Pneumatosis Cystoides Intestinalis in the Setting of Splenic Laceration, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Brooke Army Medical Center, San Antonio, TX
Introduction: Pneumatosis cystoides intestinalis (PCI) is a rare disease characterized by the presence of gaseous cysts in the intestinal wall. We present a rare case of a PCI polyp resectioned during colonoscopy in a patient with an associated splenic laceration.
Case Description/Methods: A 52-year-old female with history of class II obesity (BMI 37.4) underwent initial average risk screening colonoscopy. Advancement of the colonoscope was marked by significant angulation and looping requiring frequent repositioning and abdominal pressure. During withdrawal, five subcentimeter polyps were resected with cold snare, including one visually distinct sessile sigmoid polyp with persistent bubbling despite irrigation. After discharge, the patient reported development of abdominal pain and early satiety. Computed tomography demonstrated a grade 2 splenic laceration without perforation. The patient was monitored overnight and discharged with improving symptoms. Pathology of the aforementioned polyp was consistent with PCI, with giant cell lined cystic spaces within the lamina propria.
Discussion: Known as pneumatosis cystoides coli when limited to the colon, PCI has a range of associated etiologies. While potentially iatrogenic, associations with barotrauma during procedures, infection, or pulmonary etiologies exist. When found on imaging, discrete cystic gas collections within the bowel wall are characteristic. This contrasts with intra-abdominal free air after perforation, or linear pneumatosis following ischemia. Cysts may also be visualized endoscopically, classically appearing as grape-like clusters.
Splenic injury is a rare but established complication in colonoscopy, associated with blunt trauma or tension on the splenocolic ligament. Precipitating maneuvers include loop reduction with a stiffened colonoscope or ‘hooking’ at the splenic flexure. In PCI seen after endoscopic or surgical interventions, it is proposed that intraluminal pressurization allows gas to enter the bowel wall through mucosal defects and spread throughout the surrounding lymphatics.
A solitary polyp in the absence of imaging findings as in our cases is atypical. Given the documented association of these polyps with bowel injury, we propose a causal relationship following the patient's splenic injury during colonoscopy. While our patient was promptly diagnosed with the laceration prior to receiving histology results, when discovered, these polyps may reasonably prompt further investigation into intraprocedural complications.

Figure: Sigmoid polyp, histology consistent with pneumatosis cystoides intestinalis
Disclosures:
Matthew Schwartz indicated no relevant financial relationships.
James Francis indicated no relevant financial relationships.
Matthew Schwartz, MD, James M. Francis, DO. P0332 - A Chance Finding: Pneumatosis Cystoides Intestinalis in the Setting of Splenic Laceration, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

