Sunday Poster Session
Category: Colorectal Cancer Prevention
P0407 - Procedural and Clinical Outcomes Associated with Prior Manipulation of Large Colonic Polyps Referred for Advance Tissue Resection: A Systematic Review and Meta-Analysis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Eric Smith, MD
Baylor Scott & White Medical Center
Round Rock, TX
Presenting Author(s)
Eric Smith, MD1, Yizhong Wu, MD2, Daryl Ramai, MD, MPH, Msc3, Alexander Grieme, DO4, Christopher Ko, MD, MA5, Aasma Shaukat, MD, MPH6
1Baylor Scott & White Medical Center, Round Rock, TX; 2Baylor Scott & White Medical Center, Georgetown, TX; 3University of Utah Health, Salt Lake City, UT; 4Baylor Scott & White Medical Center, Corpus Christi, TX; 5University of Utah, Salt Lake City, UT; 6NYU Langone Health, New York, NY
Introduction: Large colorectal polyps are typically referred to specialized centers for advanced tissue resection using endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD). However, these large polyps often undergo prior resection attempts, tattooing, or biopsy during the initial colonoscopy. These procedures can cause fibrosis, leading to non-lifting lesions that are less suitable for subsequent endoscopic resection. The goal of this meta-analysis is to examine the clinical implications associated with prior polyp manipulation (PPM).
Methods: We conducted a comprehensive search of PubMed, Google Scholar, and Embase from inception to June 2024 to identify studies comparing manipulated and non-manipulated polyps undergoing advanced tissue resection. We analyzed pooled data to ascertain differences in fibrosis, en bloc resection, procedure time, use of adjunctive margin ablation, and adverse events. A random effects model was used and the data was presented using odds ratios (OR) and mean difference (MD) with 95% confidence intervals (CI).
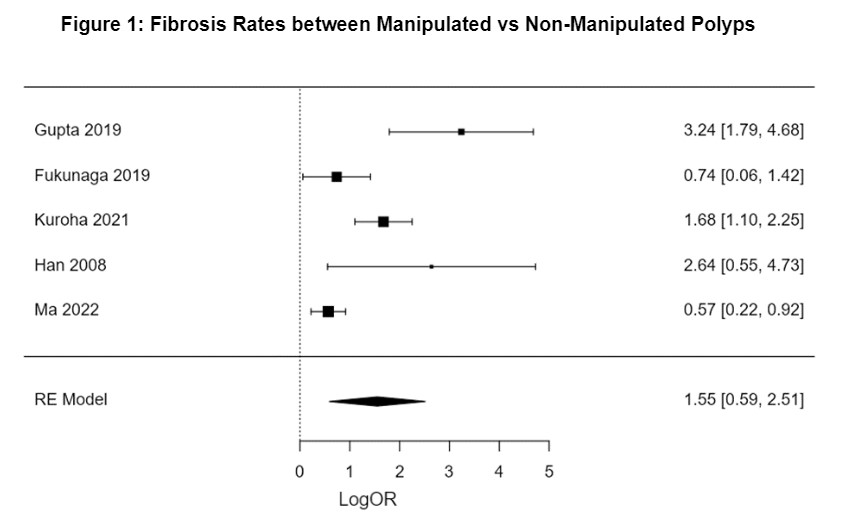
Results: Seven observational studies were included, involving 3037 polyps (1055 in the manipulated group, 1982 in the non-manipulated group). Participants were 54.5% male and 68.4 years old on average. Both manipulated and non-manipulated groups had similar polyp sizes, measuring 34.1mm and 33.9mm, respectively. The incidence of fibrosis was notably higher in the manipulated group (OR 4.7, 95% CI 1.802-12.34, p< 0.01, I2 88%). The use of adjunct margin ablation was more prevalent in the manipulated group (OR 3.8, 95% CI 1.12 - 13.4, p< 0.01, I2 89%). Procedural duration was significantly prolonged with PPM (MD 0.32, 95% CI 0.11 - 0.54, p< 0.01, I2 74%). However, there were no statistically significant differences in en bloc resection rates (p=0.31), deep mural injury (p=0.26), and overall adverse events (p=0.12). A slight trend was noted towards a higher incidence of bleeding with PPM (OR 1.3, 95% CI 0.995 - 1.69, p=0.055). Polyp recurrence rates did not differ between groups (p=0.5).
Discussion: Manipulating polyps before referral for advanced tissue resection led to higher rates of fibrosis and was linked to longer procedural times, increased use of additional therapy, and periprocedural bleeding. These results demonstrate that polyp manipulation should be discouraged, and prompt referral for definitive management should be a priority if it does occur.
Disclosures:
Eric Smith, MD1, Yizhong Wu, MD2, Daryl Ramai, MD, MPH, Msc3, Alexander Grieme, DO4, Christopher Ko, MD, MA5, Aasma Shaukat, MD, MPH6. P0407 - Procedural and Clinical Outcomes Associated with Prior Manipulation of Large Colonic Polyps Referred for Advance Tissue Resection: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Baylor Scott & White Medical Center, Round Rock, TX; 2Baylor Scott & White Medical Center, Georgetown, TX; 3University of Utah Health, Salt Lake City, UT; 4Baylor Scott & White Medical Center, Corpus Christi, TX; 5University of Utah, Salt Lake City, UT; 6NYU Langone Health, New York, NY
Introduction: Large colorectal polyps are typically referred to specialized centers for advanced tissue resection using endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD). However, these large polyps often undergo prior resection attempts, tattooing, or biopsy during the initial colonoscopy. These procedures can cause fibrosis, leading to non-lifting lesions that are less suitable for subsequent endoscopic resection. The goal of this meta-analysis is to examine the clinical implications associated with prior polyp manipulation (PPM).
Methods: We conducted a comprehensive search of PubMed, Google Scholar, and Embase from inception to June 2024 to identify studies comparing manipulated and non-manipulated polyps undergoing advanced tissue resection. We analyzed pooled data to ascertain differences in fibrosis, en bloc resection, procedure time, use of adjunctive margin ablation, and adverse events. A random effects model was used and the data was presented using odds ratios (OR) and mean difference (MD) with 95% confidence intervals (CI).
Results: Seven observational studies were included, involving 3037 polyps (1055 in the manipulated group, 1982 in the non-manipulated group). Participants were 54.5% male and 68.4 years old on average. Both manipulated and non-manipulated groups had similar polyp sizes, measuring 34.1mm and 33.9mm, respectively. The incidence of fibrosis was notably higher in the manipulated group (OR 4.7, 95% CI 1.802-12.34, p< 0.01, I2 88%). The use of adjunct margin ablation was more prevalent in the manipulated group (OR 3.8, 95% CI 1.12 - 13.4, p< 0.01, I2 89%). Procedural duration was significantly prolonged with PPM (MD 0.32, 95% CI 0.11 - 0.54, p< 0.01, I2 74%). However, there were no statistically significant differences in en bloc resection rates (p=0.31), deep mural injury (p=0.26), and overall adverse events (p=0.12). A slight trend was noted towards a higher incidence of bleeding with PPM (OR 1.3, 95% CI 0.995 - 1.69, p=0.055). Polyp recurrence rates did not differ between groups (p=0.5).
Discussion: Manipulating polyps before referral for advanced tissue resection led to higher rates of fibrosis and was linked to longer procedural times, increased use of additional therapy, and periprocedural bleeding. These results demonstrate that polyp manipulation should be discouraged, and prompt referral for definitive management should be a priority if it does occur.
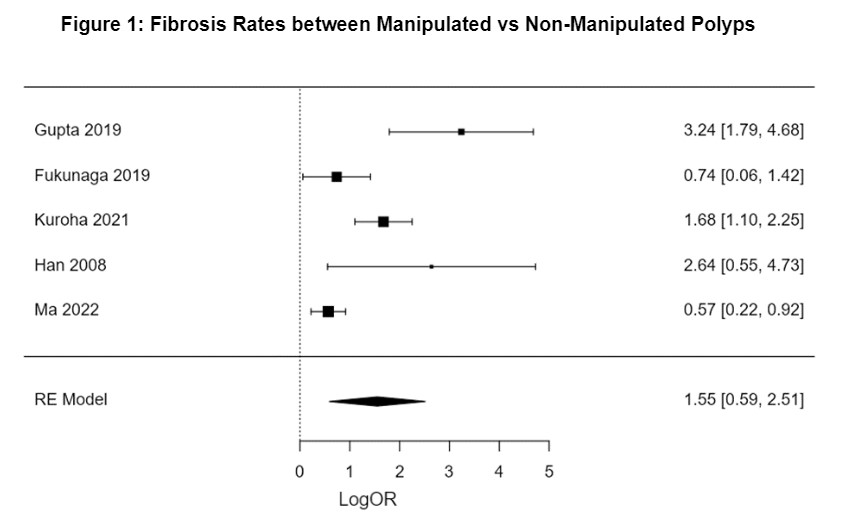
Figure: Fibrosis Rates between Manipulated vs Non-Manipulated Polyps
Disclosures:
Eric Smith indicated no relevant financial relationships.
Yizhong Wu indicated no relevant financial relationships.
Daryl Ramai indicated no relevant financial relationships.
Alexander Grieme indicated no relevant financial relationships.
Christopher Ko indicated no relevant financial relationships.
Aasma Shaukat: iterative health; Freenome – Consultant.
Eric Smith, MD1, Yizhong Wu, MD2, Daryl Ramai, MD, MPH, Msc3, Alexander Grieme, DO4, Christopher Ko, MD, MA5, Aasma Shaukat, MD, MPH6. P0407 - Procedural and Clinical Outcomes Associated with Prior Manipulation of Large Colonic Polyps Referred for Advance Tissue Resection: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
