Sunday Poster Session
Category: Colorectal Cancer Prevention
P0408 - Decreasing Post-Colonoscopy Colon Cancer Rates Correlate With Improvements in Adenoma Detection Rate and Withdrawal Time
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Megan Price, BS
University of Illinois College of Medicine
Loves Park, IL
Presenting Author(s)
Aaron Shiels, MD1, Megan Price, BS2, Ellie Kirane, BS3
1Rockford Gastroenterology Associates, Rockford, IL; 2University of Illinois College of Medicine, Loves Park, IL; 3Northern Illinois University, Bowling Green, OH
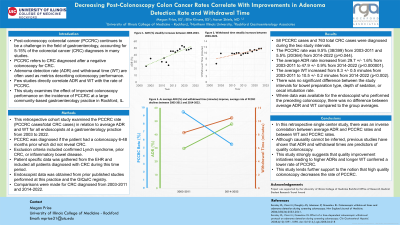
Introduction: Post-colonoscopy colorectal cancer (PCCRC) continues to be a challenge in the field of gastroenterology, accounting for 5-15% of the colorectal cancer (CRC) diagnoses in many studies. PCCRC refers to CRC diagnosed after a negative colonoscopy for CRC. Adenoma detection rate (ADR) and withdrawal time (WT) are often used as metrics describing colonoscopy performance. Few studies directly correlate ADR and WT with the rate of PCCRC. This study examines the effect of improved colonoscopy performance on the incidence of PCCRC at a large community-based gastroenterology practice.
Methods: This retrospective cohort study examined the PCCRC rate (PCCRC cases/total CRC cases) in relation to average ADR and WT for all endoscopists at a gastroenterology practice from 2003 to 2022. PCCRC was diagnosed if the patient had a colonoscopy 6-48 months prior which did not reveal CRC. Exclusion criteria included confirmed Lynch syndrome, prior CRC, or inflammatory bowel disease. Patient specific data was gathered from the EHR and included all patients diagnosed with CRC during this time period. Endoscopist data was obtained from prior published studies performed at this practice and the GIQuIC registry. Comparisons were made for CRC diagnosed from 2003-2011 and 2014-2022.
Results: 58 PCCRC cases and 763 total CRC cases were diagnosed during the two study intervals. The PCCRC rate was 9.5% (38/399) from 2003-2011 and 5.5% (20/364) from 2014-2022 (p=0.044). The average ADR rate increased from 29.7 +/- 1.6% from 2003-2011 to 47.9 +/- 0.9% from 2014-2022 (p< 0.000001). The average WT increased from 8.3 +/- 0.5 minutes from 2003-2011 to 10.5 +/- 0.2 minutes from 2014-2022 (p< 0.002). There was no significant difference between the study intervals for bowel preparation type, depth of sedation, or cecal intubation rate. Where data was available for the endoscopist who performed the preceding colonoscopy, there was no difference between average ADR and WT compared to the group averages.
Discussion: In this retrospective single center study, there was an inverse correlation between average ADR and PCCRC rates and a direct correlation between WT and PCCRC rates. Although causality cannot be inferred, previous studies have shown that ADR and withdrawal times are predictors of quality colonoscopy. This study strongly suggests that quality improvement initiatives leading to higher ADRs and longer WT confer a lower rate of PCCRC. High quality colonoscopy is essential in preventing PCCRC.
Disclosures:
Aaron Shiels, MD1, Megan Price, BS2, Ellie Kirane, BS3. P0408 - Decreasing Post-Colonoscopy Colon Cancer Rates Correlate With Improvements in Adenoma Detection Rate and Withdrawal Time, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Rockford Gastroenterology Associates, Rockford, IL; 2University of Illinois College of Medicine, Loves Park, IL; 3Northern Illinois University, Bowling Green, OH
Introduction: Post-colonoscopy colorectal cancer (PCCRC) continues to be a challenge in the field of gastroenterology, accounting for 5-15% of the colorectal cancer (CRC) diagnoses in many studies. PCCRC refers to CRC diagnosed after a negative colonoscopy for CRC. Adenoma detection rate (ADR) and withdrawal time (WT) are often used as metrics describing colonoscopy performance. Few studies directly correlate ADR and WT with the rate of PCCRC. This study examines the effect of improved colonoscopy performance on the incidence of PCCRC at a large community-based gastroenterology practice.
Methods: This retrospective cohort study examined the PCCRC rate (PCCRC cases/total CRC cases) in relation to average ADR and WT for all endoscopists at a gastroenterology practice from 2003 to 2022. PCCRC was diagnosed if the patient had a colonoscopy 6-48 months prior which did not reveal CRC. Exclusion criteria included confirmed Lynch syndrome, prior CRC, or inflammatory bowel disease. Patient specific data was gathered from the EHR and included all patients diagnosed with CRC during this time period. Endoscopist data was obtained from prior published studies performed at this practice and the GIQuIC registry. Comparisons were made for CRC diagnosed from 2003-2011 and 2014-2022.
Results: 58 PCCRC cases and 763 total CRC cases were diagnosed during the two study intervals. The PCCRC rate was 9.5% (38/399) from 2003-2011 and 5.5% (20/364) from 2014-2022 (p=0.044). The average ADR rate increased from 29.7 +/- 1.6% from 2003-2011 to 47.9 +/- 0.9% from 2014-2022 (p< 0.000001). The average WT increased from 8.3 +/- 0.5 minutes from 2003-2011 to 10.5 +/- 0.2 minutes from 2014-2022 (p< 0.002). There was no significant difference between the study intervals for bowel preparation type, depth of sedation, or cecal intubation rate. Where data was available for the endoscopist who performed the preceding colonoscopy, there was no difference between average ADR and WT compared to the group averages.
Discussion: In this retrospective single center study, there was an inverse correlation between average ADR and PCCRC rates and a direct correlation between WT and PCCRC rates. Although causality cannot be inferred, previous studies have shown that ADR and withdrawal times are predictors of quality colonoscopy. This study strongly suggests that quality improvement initiatives leading to higher ADRs and longer WT confer a lower rate of PCCRC. High quality colonoscopy is essential in preventing PCCRC.
Disclosures:
Aaron Shiels indicated no relevant financial relationships.
Megan Price indicated no relevant financial relationships.
Ellie Kirane indicated no relevant financial relationships.
Aaron Shiels, MD1, Megan Price, BS2, Ellie Kirane, BS3. P0408 - Decreasing Post-Colonoscopy Colon Cancer Rates Correlate With Improvements in Adenoma Detection Rate and Withdrawal Time, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
