Sunday Poster Session
Category: Colorectal Cancer Prevention
P0413 - Clearing the Way: Improving Inpatient Colonoscopy Bowel Preparation
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Neel Shah, MD
Baylor Scott & White Medical Center
Bay City, TX
Presenting Author(s)
Neel Shah, MD1, Eric Smith, MD1, Yizhong Wu, MD2, Sanjay Prasad, MD1, Manuel Garza, MD1, Harold Averill, DO1, Wasay A. Mohajir, DO1, Michael Quinton, MD1, Ravi Janumpally, MD1, Judith Amaning, MD1
1Baylor Scott & White Medical Center, Round Rock, TX; 2Baylor Scott & White Medical Center, Georgetown, TX
Introduction: The quality of bowel preparation must be optimal for good procedural outcomes, patient experience, and maximizing healthcare efficiency. It is well documented that inpatient bowel preps are less quality when compared to outpatient bowel preps. Poor bowel prep has been associated with up to 30% increase in hospitalization cost, delayed diagnostics, longer hospital stays, and often repeat colonoscopies.1 Our quality improvement project aimed to improve inpatient bowel preps using nursing and patient education and an improved bowel prep order set.
Methods: We defined inadequate bowel prep as a canceled colonoscopy due to poor prep, prep described as “poor” or “inadequate” in the procedure note, or Boston Bowel Prep Score (BBPS) < 6. Stage 1 of our intervention implemented nursing training and an educational pamphlet for patients. The second stage of our intervention added a new order set in the electronic medical record for inpatient colonoscopies. The order set included free text with information on troubleshooting Golightly tolerability (chill solution, add Crystal light, drink with a straw, give MiraLAX if remains intolerable), instructions to keep commode at bedside, a description of clear bowel movements, as well as a prompt to request enema the day of procedure if unclear bowel movement.
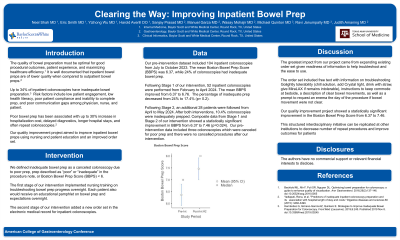
Results: Our pre-intervention dataset included 104 inpatient colonoscopies from July to October 2023. The mean Boston Bowel Prep Score (BBPS) was 6.37, while 24% of colonoscopies had inadequate bowel prep. Following Stage 1 of our intervention, 52 inpatient colonoscopies were performed from February to April 2024. The mean BBPS improved from 6.37 to 6.76. The percentage of inadequate prep decreased from 24% to 17.4% (p= 0.2). Following Stage 2, an additional 28 patients were followed from April to May 2024. After both interventions, 10.4% of colonoscopies were inadequately prepped. Composite data from Stage 1 and Stage 2 of our intervention showed a statistically significant improvement in BBPS from 6.37 to 7.46 (p=0.024). Our pre-intervention data included three colonoscopies which were canceled for poor prep and there were no cancelled procedures post-intervention.
Discussion: Our quality improvement project shows that the quality of inpatient bowel prep can be improved through nursing and patient education and an improved order set.
Reference:
1. Kingsley, James, et al. "Cost effectiveness of screening colonoscopy depends on adequate bowel preparation rates–a modeling study." PloS one 11.12 (2016)
Disclosures:
Neel Shah, MD1, Eric Smith, MD1, Yizhong Wu, MD2, Sanjay Prasad, MD1, Manuel Garza, MD1, Harold Averill, DO1, Wasay A. Mohajir, DO1, Michael Quinton, MD1, Ravi Janumpally, MD1, Judith Amaning, MD1. P0413 - Clearing the Way: Improving Inpatient Colonoscopy Bowel Preparation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Baylor Scott & White Medical Center, Round Rock, TX; 2Baylor Scott & White Medical Center, Georgetown, TX
Introduction: The quality of bowel preparation must be optimal for good procedural outcomes, patient experience, and maximizing healthcare efficiency. It is well documented that inpatient bowel preps are less quality when compared to outpatient bowel preps. Poor bowel prep has been associated with up to 30% increase in hospitalization cost, delayed diagnostics, longer hospital stays, and often repeat colonoscopies.1 Our quality improvement project aimed to improve inpatient bowel preps using nursing and patient education and an improved bowel prep order set.
Methods: We defined inadequate bowel prep as a canceled colonoscopy due to poor prep, prep described as “poor” or “inadequate” in the procedure note, or Boston Bowel Prep Score (BBPS) < 6. Stage 1 of our intervention implemented nursing training and an educational pamphlet for patients. The second stage of our intervention added a new order set in the electronic medical record for inpatient colonoscopies. The order set included free text with information on troubleshooting Golightly tolerability (chill solution, add Crystal light, drink with a straw, give MiraLAX if remains intolerable), instructions to keep commode at bedside, a description of clear bowel movements, as well as a prompt to request enema the day of procedure if unclear bowel movement.
Results: Our pre-intervention dataset included 104 inpatient colonoscopies from July to October 2023. The mean Boston Bowel Prep Score (BBPS) was 6.37, while 24% of colonoscopies had inadequate bowel prep. Following Stage 1 of our intervention, 52 inpatient colonoscopies were performed from February to April 2024. The mean BBPS improved from 6.37 to 6.76. The percentage of inadequate prep decreased from 24% to 17.4% (p= 0.2). Following Stage 2, an additional 28 patients were followed from April to May 2024. After both interventions, 10.4% of colonoscopies were inadequately prepped. Composite data from Stage 1 and Stage 2 of our intervention showed a statistically significant improvement in BBPS from 6.37 to 7.46 (p=0.024). Our pre-intervention data included three colonoscopies which were canceled for poor prep and there were no cancelled procedures post-intervention.
Discussion: Our quality improvement project shows that the quality of inpatient bowel prep can be improved through nursing and patient education and an improved order set.
Reference:
1. Kingsley, James, et al. "Cost effectiveness of screening colonoscopy depends on adequate bowel preparation rates–a modeling study." PloS one 11.12 (2016)
Disclosures:
Neel Shah indicated no relevant financial relationships.
Eric Smith indicated no relevant financial relationships.
Yizhong Wu indicated no relevant financial relationships.
Sanjay Prasad indicated no relevant financial relationships.
Manuel Garza indicated no relevant financial relationships.
Harold Averill indicated no relevant financial relationships.
Wasay Mohajir indicated no relevant financial relationships.
Michael Quinton indicated no relevant financial relationships.
Ravi Janumpally indicated no relevant financial relationships.
Judith Amaning indicated no relevant financial relationships.
Neel Shah, MD1, Eric Smith, MD1, Yizhong Wu, MD2, Sanjay Prasad, MD1, Manuel Garza, MD1, Harold Averill, DO1, Wasay A. Mohajir, DO1, Michael Quinton, MD1, Ravi Janumpally, MD1, Judith Amaning, MD1. P0413 - Clearing the Way: Improving Inpatient Colonoscopy Bowel Preparation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
