Sunday Poster Session
Category: Colorectal Cancer Prevention
P0416 - Assessing the Use of Fecal Occult Blood Tests in a Community Hospital: Phase Two
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
Sarah Singh, MD
West Virginia University Camden Clark Medical Center
Parkersburg, WV
Presenting Author(s)
Sarah Singh, MD1, Winnie Roy, MD, MS1, Michael Iannetti, MD2
1West Virginia University Camden Clark Medical Center, Parkersburg, WV; 2Charleston Area Medical Center, Charleston, WV
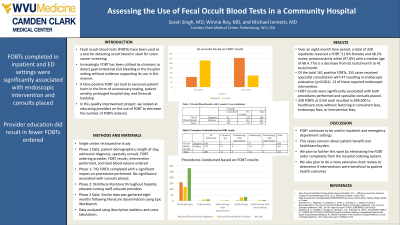
Introduction: Fecal occult blood tests (FOBT) have been used as a tool for detecting occult blood in stool for colon cancer screening. Increasingly, FOBT has been utilized by clinicians to detect gastrointestinal (GI) bleeding in the hospital setting without evidence supporting its use in this manner. Two studies looked at the use of FOBTs in the community hospital setting and both found that FOBTs were used for non-evidence-based indications and did not offer any clinical benefit. Furthermore, a false positive FOBT can lead to excessive patient harm in the form of unnecessary testing, patient anxiety, prolonged hospital stay, and financial hardship.
Methods: During phase one of this study, we gathered patient data using search criteria including patient demographics, length of stay, admission diagnosis, specialty consulted, FOBT ordering provider, FOBT results, intervention performed, and total blood volume ordered. These data revealed that over a one-year period, FOBT did have a significant impact on whether an invasive intervention, such as colonoscopy or gastroscopy, was performed but not whether specialist consult was placed. We then distributed our findings throughout the hospital to educate clinical staff on the appropriate use of FOBT testing. Data was recollected after eight months.
Results: During this time, 328 FOBTs were ordered on admitted patients with a mean age of 68.4 years; 51.8% females and 48.2% males; predominantly whites 97.6% and African American 2.1%. This is fewer than the 742 FOBTs ordered during phase one. Of the 328, 161 FOBT results were positive and 166 were negative. Specialty consults to Gastroenterology or General surgery were placed on 155 of these cases, with 47 resulting in endoscopic evaluation. Endoscopic intervention was only carried out in 13 of the 47 procedures. Similar to phase one, FOBT results had a significant impact on endoscopic evaluation. However, they now also had a significant impact on the placement of specialist consults. Fecal occult blood testing for these 328 patients added a total of $49,500 to healthcare costs.
Discussion: Our attempt to educate providers resulted in fewer FOBTs ordered. Despite questionable benefits and literature advising against its use, FOBTs have continued to appear in the inpatient setting. In an effort to further reduce the number of FOBTs ordered, we plan to remove the order completely from our electronic health record.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sarah Singh, MD1, Winnie Roy, MD, MS1, Michael Iannetti, MD2. P0416 - Assessing the Use of Fecal Occult Blood Tests in a Community Hospital: Phase Two, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1West Virginia University Camden Clark Medical Center, Parkersburg, WV; 2Charleston Area Medical Center, Charleston, WV
Introduction: Fecal occult blood tests (FOBT) have been used as a tool for detecting occult blood in stool for colon cancer screening. Increasingly, FOBT has been utilized by clinicians to detect gastrointestinal (GI) bleeding in the hospital setting without evidence supporting its use in this manner. Two studies looked at the use of FOBTs in the community hospital setting and both found that FOBTs were used for non-evidence-based indications and did not offer any clinical benefit. Furthermore, a false positive FOBT can lead to excessive patient harm in the form of unnecessary testing, patient anxiety, prolonged hospital stay, and financial hardship.
Methods: During phase one of this study, we gathered patient data using search criteria including patient demographics, length of stay, admission diagnosis, specialty consulted, FOBT ordering provider, FOBT results, intervention performed, and total blood volume ordered. These data revealed that over a one-year period, FOBT did have a significant impact on whether an invasive intervention, such as colonoscopy or gastroscopy, was performed but not whether specialist consult was placed. We then distributed our findings throughout the hospital to educate clinical staff on the appropriate use of FOBT testing. Data was recollected after eight months.
Results: During this time, 328 FOBTs were ordered on admitted patients with a mean age of 68.4 years; 51.8% females and 48.2% males; predominantly whites 97.6% and African American 2.1%. This is fewer than the 742 FOBTs ordered during phase one. Of the 328, 161 FOBT results were positive and 166 were negative. Specialty consults to Gastroenterology or General surgery were placed on 155 of these cases, with 47 resulting in endoscopic evaluation. Endoscopic intervention was only carried out in 13 of the 47 procedures. Similar to phase one, FOBT results had a significant impact on endoscopic evaluation. However, they now also had a significant impact on the placement of specialist consults. Fecal occult blood testing for these 328 patients added a total of $49,500 to healthcare costs.
Discussion: Our attempt to educate providers resulted in fewer FOBTs ordered. Despite questionable benefits and literature advising against its use, FOBTs have continued to appear in the inpatient setting. In an effort to further reduce the number of FOBTs ordered, we plan to remove the order completely from our electronic health record.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sarah Singh indicated no relevant financial relationships.
Winnie Roy indicated no relevant financial relationships.
Michael Iannetti indicated no relevant financial relationships.
Sarah Singh, MD1, Winnie Roy, MD, MS1, Michael Iannetti, MD2. P0416 - Assessing the Use of Fecal Occult Blood Tests in a Community Hospital: Phase Two, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
