Sunday Poster Session
Category: Colorectal Cancer Prevention
P0417 - Associations Between Sociodemographic Characteristics and Colorectal Cancer Screening in a Large VA Cohort, 2002-2018
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Joshua D. Kirschenbaum, MD
Tufts
Boston, MA
Presenting Author(s)
Joshua D. Kirschenbaum, MD1, Yingzhi Qian, 2, Shinjini Nandi, PhD3, Simona Kwon, 4, Ann G.. Zauber, PhD5, Jason A. Dominitz, MD, MHS6, Scott Sherman, MD, MPH4, Peter S.. Liang, MD, MPH7
1Tufts, Boston, MA; 2New York University, New York, NY; 3New York University Langone Health, Bozeman, MT; 4NYU Grossman School of Medicine, New York, NY; 5Memorial Sloan Kettering Cancer Center, New York, NY; 6Veterans Health Administration, Bellevue, WA; 7NYU Langone Health, New York, NY
Introduction: Associations between patient sociodemographic factors and colorectal cancer (CRC) screening adherence over time have not been fully assessed. We examined these relationships using a large cohort in the Veterans Health Administration (VA) from 2002 to 2018.
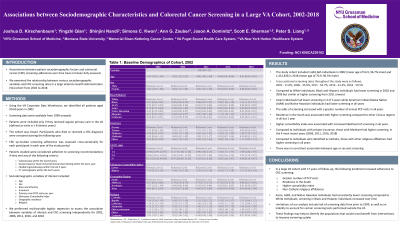
Methods: We identified all individuals aged 50-60 years in 2002 who received regular primary care at the VA through 2018—defined as visits in at least 8 distinct years. Those who died or received a CRC diagnosis were censored. Variables of interest included age, sex, race/ethnicity, insurance, primary care (PCP) visits per year, Elixhauser Comorbidity Index, geographic residence, and religion. We performed multivariable logistic regression to assess the association between variables of interest and CRC screening independently for 2002, 2006, 2011, 2016, and 2018. Screening data were available since 1999, and individuals were considered adherent in a calendar year if they completed screening any time during that year.
Results: The cohort included 1,681,665 individuals in 2002 and 1,431,828 in 2018. On logistic regression, compared to White individuals, Black and Hispanic individuals had lower screening in 2002 and 2006 but similar or higher screening from 2011 onward; Asian individuals had lower screening in 4 of 5 years while American Indian/Alaska Native (AIAN) and Native Hawaiian individuals had lower screening in all years. Odds of screening increased with a greater number of annual PCP visits in all years. Residence in the South was associated with higher screening compared to other Census regions in all but 1 year. Higher comorbidity index was associated with screening in all years. Compared to individuals with private insurance, those with Medicare had higher screening in the 4 most recent years. Compared to individuals who identified as Catholic, those with other religious affiliations had higher screening in all years. There was no consistent association between age or sex and screening.
Discussion: In a large VA cohort with 17 years of follow-up, greater number of PCP visits, residence in the South, higher comorbidity index, and certain religious affiliations consistently predicted increased adherence to CRC screening. Asian, AIAN, and Native Hawaiian individuals had consistently lower screening compared to White individuals, while screening in Black and Hispanic individuals increased over time. These findings may help to identify populations who would benefit from interventions to improve screening uptake.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Joshua D. Kirschenbaum, MD1, Yingzhi Qian, 2, Shinjini Nandi, PhD3, Simona Kwon, 4, Ann G.. Zauber, PhD5, Jason A. Dominitz, MD, MHS6, Scott Sherman, MD, MPH4, Peter S.. Liang, MD, MPH7. P0417 - Associations Between Sociodemographic Characteristics and Colorectal Cancer Screening in a Large VA Cohort, 2002-2018, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Tufts, Boston, MA; 2New York University, New York, NY; 3New York University Langone Health, Bozeman, MT; 4NYU Grossman School of Medicine, New York, NY; 5Memorial Sloan Kettering Cancer Center, New York, NY; 6Veterans Health Administration, Bellevue, WA; 7NYU Langone Health, New York, NY
Introduction: Associations between patient sociodemographic factors and colorectal cancer (CRC) screening adherence over time have not been fully assessed. We examined these relationships using a large cohort in the Veterans Health Administration (VA) from 2002 to 2018.
Methods: We identified all individuals aged 50-60 years in 2002 who received regular primary care at the VA through 2018—defined as visits in at least 8 distinct years. Those who died or received a CRC diagnosis were censored. Variables of interest included age, sex, race/ethnicity, insurance, primary care (PCP) visits per year, Elixhauser Comorbidity Index, geographic residence, and religion. We performed multivariable logistic regression to assess the association between variables of interest and CRC screening independently for 2002, 2006, 2011, 2016, and 2018. Screening data were available since 1999, and individuals were considered adherent in a calendar year if they completed screening any time during that year.
Results: The cohort included 1,681,665 individuals in 2002 and 1,431,828 in 2018. On logistic regression, compared to White individuals, Black and Hispanic individuals had lower screening in 2002 and 2006 but similar or higher screening from 2011 onward; Asian individuals had lower screening in 4 of 5 years while American Indian/Alaska Native (AIAN) and Native Hawaiian individuals had lower screening in all years. Odds of screening increased with a greater number of annual PCP visits in all years. Residence in the South was associated with higher screening compared to other Census regions in all but 1 year. Higher comorbidity index was associated with screening in all years. Compared to individuals with private insurance, those with Medicare had higher screening in the 4 most recent years. Compared to individuals who identified as Catholic, those with other religious affiliations had higher screening in all years. There was no consistent association between age or sex and screening.
Discussion: In a large VA cohort with 17 years of follow-up, greater number of PCP visits, residence in the South, higher comorbidity index, and certain religious affiliations consistently predicted increased adherence to CRC screening. Asian, AIAN, and Native Hawaiian individuals had consistently lower screening compared to White individuals, while screening in Black and Hispanic individuals increased over time. These findings may help to identify populations who would benefit from interventions to improve screening uptake.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Joshua Kirschenbaum indicated no relevant financial relationships.
Yingzhi Qian indicated no relevant financial relationships.
Shinjini Nandi indicated no relevant financial relationships.
Simona Kwon indicated no relevant financial relationships.
Ann Zauber indicated no relevant financial relationships.
Jason Dominitz indicated no relevant financial relationships.
Scott Sherman indicated no relevant financial relationships.
Peter Liang: Freenome – Grant/Research Support. Guardant Health – Advisory Committee/Board Member. Natera – Advisory Committee/Board Member.
Joshua D. Kirschenbaum, MD1, Yingzhi Qian, 2, Shinjini Nandi, PhD3, Simona Kwon, 4, Ann G.. Zauber, PhD5, Jason A. Dominitz, MD, MHS6, Scott Sherman, MD, MPH4, Peter S.. Liang, MD, MPH7. P0417 - Associations Between Sociodemographic Characteristics and Colorectal Cancer Screening in a Large VA Cohort, 2002-2018, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
