Sunday Poster Session
Category: Colorectal Cancer Prevention
P0418 - Predictors for No-Show After Endoscopic Mucosal Resection of Colorectal Polyps: Insights from a Retrospective Veterans Affairs Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Hayden E. Rotramel, MD
SSM Health St. Louis University Hospital
St. Louis, MO
Presenting Author(s)
Mahmoud Y. Madi, MD1, Hayden Rotramel, MD2, Yassine Kilani, MD1, Michelle Baliss, DO1, Jill E. Elwing, MD3, Gregory Sayuk, MD3, Ahmad Najdat Bazarbashi, MD4
1SSM Health Saint Louis University Hospital, St. Louis, MO; 2SSM Health St. Louis University Hospital, St. Louis, MO; 3Washington University School of Medicine in St. Louis, St. Louis, MO; 4Washington University School of Medicine in St. Louis / Barnes-Jewish Hospital, St. Louis, MO
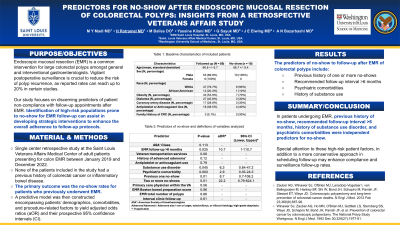
Introduction: Endoscopic mucosal resection (EMR) is a common intervention for large colorectal polyps amongst general and interventional gastroenterologists. Vigilant postoperative surveillance is crucial to reduce the risk of polyp recurrence, as reported rates can reach up to 20% in certain studies. Our study focuses on discerning predictors of patient non-compliance with follow-up appointments after EMR. Identification of high-risk populations prone to no-show for EMR follow-up can assist in developing strategic interventions to enhance the overall adherence to post-EMR follow-up protocols.
Methods: We conducted a single center retrospective study of adult patients presenting for colon EMR between January 2019 and December 2022. The primary outcome was the no-show rates for patients who previously underwent EMR. A predictive model was then constructed encompassing patients’ demographics, comorbidities, and procedure-related factors to yield adjusted odds ratios (aOR) and their prospective 95% confidence intervals (CI).
Results: A total of sixty-nine (N=69) patients (mean age 66.8 +/- 7 years, 8.7% females, 18.8% African American) met the inclusion criteria of our study. Baseline characteristics are outlined in Table 1. The adherence rate at the recommended interval for surveillance colonoscopy was 85.5% (59/69). Only ten patients (14.5%) failed to attend their follow-up appointment and were regarded as “no-shows”. The predictors of no-show with their aOR and 95% CI in descending order included previous history of one or more no-shows (3.8, 1.7-8.5, p=0.002), recommended follow-up interval greater than 6 months (3.5, 1.1-12.5, p=0.04), psychiatric comorbidities (2.8, 1.7-4.6, p=0.002), and history of substance use (2.7, 1.8-6.0, p=0.03). Patients with family history of colorectal cancer were more likely to no-show in our study (30.0% no-show rate vs 5.1%, p=0.034). The use of veteran transportation services showed a trend to decrease the rates of no-show without reaching statistical significance (7.0% no-show rate vs 14.5%, p=0.06).
Discussion: In patients undergoing EMR, previous history of no-show, recommended follow-up interval greater than 6 months, history of substance use disorder, and psychiatric comorbidities were independent predictors for no-show. Special attention to these high-risk patient factors, in addition to a more conservative approach in scheduling follow-up may enhance compliance and surveillance follow-up rates.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mahmoud Y. Madi, MD1, Hayden Rotramel, MD2, Yassine Kilani, MD1, Michelle Baliss, DO1, Jill E. Elwing, MD3, Gregory Sayuk, MD3, Ahmad Najdat Bazarbashi, MD4. P0418 - Predictors for No-Show After Endoscopic Mucosal Resection of Colorectal Polyps: Insights from a Retrospective Veterans Affairs Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1SSM Health Saint Louis University Hospital, St. Louis, MO; 2SSM Health St. Louis University Hospital, St. Louis, MO; 3Washington University School of Medicine in St. Louis, St. Louis, MO; 4Washington University School of Medicine in St. Louis / Barnes-Jewish Hospital, St. Louis, MO
Introduction: Endoscopic mucosal resection (EMR) is a common intervention for large colorectal polyps amongst general and interventional gastroenterologists. Vigilant postoperative surveillance is crucial to reduce the risk of polyp recurrence, as reported rates can reach up to 20% in certain studies. Our study focuses on discerning predictors of patient non-compliance with follow-up appointments after EMR. Identification of high-risk populations prone to no-show for EMR follow-up can assist in developing strategic interventions to enhance the overall adherence to post-EMR follow-up protocols.
Methods: We conducted a single center retrospective study of adult patients presenting for colon EMR between January 2019 and December 2022. The primary outcome was the no-show rates for patients who previously underwent EMR. A predictive model was then constructed encompassing patients’ demographics, comorbidities, and procedure-related factors to yield adjusted odds ratios (aOR) and their prospective 95% confidence intervals (CI).
Results: A total of sixty-nine (N=69) patients (mean age 66.8 +/- 7 years, 8.7% females, 18.8% African American) met the inclusion criteria of our study. Baseline characteristics are outlined in Table 1. The adherence rate at the recommended interval for surveillance colonoscopy was 85.5% (59/69). Only ten patients (14.5%) failed to attend their follow-up appointment and were regarded as “no-shows”. The predictors of no-show with their aOR and 95% CI in descending order included previous history of one or more no-shows (3.8, 1.7-8.5, p=0.002), recommended follow-up interval greater than 6 months (3.5, 1.1-12.5, p=0.04), psychiatric comorbidities (2.8, 1.7-4.6, p=0.002), and history of substance use (2.7, 1.8-6.0, p=0.03). Patients with family history of colorectal cancer were more likely to no-show in our study (30.0% no-show rate vs 5.1%, p=0.034). The use of veteran transportation services showed a trend to decrease the rates of no-show without reaching statistical significance (7.0% no-show rate vs 14.5%, p=0.06).
Discussion: In patients undergoing EMR, previous history of no-show, recommended follow-up interval greater than 6 months, history of substance use disorder, and psychiatric comorbidities were independent predictors for no-show. Special attention to these high-risk patient factors, in addition to a more conservative approach in scheduling follow-up may enhance compliance and surveillance follow-up rates.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mahmoud Madi indicated no relevant financial relationships.
Hayden Rotramel indicated no relevant financial relationships.
Yassine Kilani indicated no relevant financial relationships.
Michelle Baliss indicated no relevant financial relationships.
Jill Elwing indicated no relevant financial relationships.
Gregory Sayuk indicated no relevant financial relationships.
Ahmad Najdat Bazarbashi indicated no relevant financial relationships.
Mahmoud Y. Madi, MD1, Hayden Rotramel, MD2, Yassine Kilani, MD1, Michelle Baliss, DO1, Jill E. Elwing, MD3, Gregory Sayuk, MD3, Ahmad Najdat Bazarbashi, MD4. P0418 - Predictors for No-Show After Endoscopic Mucosal Resection of Colorectal Polyps: Insights from a Retrospective Veterans Affairs Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
