Sunday Poster Session
Category: Colorectal Cancer Prevention
P0429 - The Impact of Real Time Artificial Intelligence Enhanced Colonoscopy: A One Year Performance Review
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Kapil D. Nayar, MD
Mayo Clinic
Griffin
Presenting Author(s)
Kapil D. Nayar, MD1, Abdelrahman Yakout, MD2, Bakheet Nader, MBBCh, PhD2, Patrick S. Sanchez, 2, Yan Yan, MBBS, PhD2, Yuting Huang, MBBS, PhD2, Manar Al Jawish, MD2, Michael B. Wallace, MD, MPH2, Vivek Kumbhari, MBChB, PhD2
1Mayo Clinic, Griffin, GA; 2Mayo Clinic, Jacksonville, FL
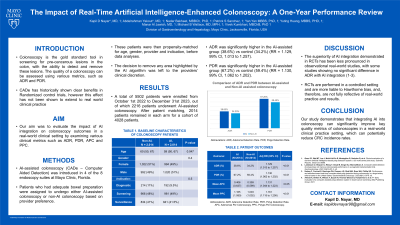
Introduction: Colonoscopy is the gold standard tool for screening for pre-cancerous lesions in the colon with the ability to detect and remove these lesions. The quality of a colonoscopy can be assessed using various metrics, the most important of which is Adenoma Detection Rate (ADR), which correlates inversely with colorectal cancer incidence and mortality. Combining colonoscopy with AI aims to further enhance the detection rates of pre-cancerous lesions and optimize colorectal cancer prevention. Our study evaluates the impact of AI integration on colonoscopy outcomes in a real-world clinical setting.
Methods: We prospectively collected data from all colonoscopies performed with AI-assistance from a newly FDA approved computer aided detection (CADe) system between October 2022 and December 2023 at Mayo Clinic in Florida. AI-assisted colonoscopy is implemented in 4 out of 8 endoscopy rooms to which patients are assigned randomly based on availability and scheduling. Polyps were identified andanalyzed by standard histopathology and classified as adenoma or non-adenoma based on standard criteria. Propensity score matching was performed to match AI cases with non-AI controls based on age, gender, provider, and indications (screening, surveillance, and diagnostic) in a (1:1) ratio.
Adenoma Detection Rate (ADR), Polyp Detection Rate (PDR), Polyps per Colonoscopy (PPC), and Adenoma Per Colonoscopy (APC) in AI cases and non-AI controls were then calculated and compared.
Results: The final analysis included 4028 patients (2014 cases, 2014 controls) with adequate bowelpreparation.
ADR was significantly higher in AI assisted group (38.6%) vs control (34.2%) (RR = 1.129, 99% CI, 1.013 to 1.257). PDR was also significantly higher in AI assisted group (67.2%) vs control (59.4%) (RR = 1.130, 99% CI, 1.062 to 1.202). Mean APC was significantly higher in AI group (0.406) vs control (0.359) (RR = 1.131, 95% CI, 1.046 to 1.223). PPC was also significantly higher in AI assisted group (5.276) vs control (4.452) (RR = 1.161, 99% CI, 1.115 to 1.208).
Discussion: Our study shows that AI-assisted colonoscopy is associated with an increased ADR, PDR, PPC, and APC ratios. The higher ADR translates to lower rates of interval colorectal cancer and improved patient outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kapil D. Nayar, MD1, Abdelrahman Yakout, MD2, Bakheet Nader, MBBCh, PhD2, Patrick S. Sanchez, 2, Yan Yan, MBBS, PhD2, Yuting Huang, MBBS, PhD2, Manar Al Jawish, MD2, Michael B. Wallace, MD, MPH2, Vivek Kumbhari, MBChB, PhD2. P0429 - The Impact of Real Time Artificial Intelligence Enhanced Colonoscopy: A One Year Performance Review, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mayo Clinic, Griffin, GA; 2Mayo Clinic, Jacksonville, FL
Introduction: Colonoscopy is the gold standard tool for screening for pre-cancerous lesions in the colon with the ability to detect and remove these lesions. The quality of a colonoscopy can be assessed using various metrics, the most important of which is Adenoma Detection Rate (ADR), which correlates inversely with colorectal cancer incidence and mortality. Combining colonoscopy with AI aims to further enhance the detection rates of pre-cancerous lesions and optimize colorectal cancer prevention. Our study evaluates the impact of AI integration on colonoscopy outcomes in a real-world clinical setting.
Methods: We prospectively collected data from all colonoscopies performed with AI-assistance from a newly FDA approved computer aided detection (CADe) system between October 2022 and December 2023 at Mayo Clinic in Florida. AI-assisted colonoscopy is implemented in 4 out of 8 endoscopy rooms to which patients are assigned randomly based on availability and scheduling. Polyps were identified andanalyzed by standard histopathology and classified as adenoma or non-adenoma based on standard criteria. Propensity score matching was performed to match AI cases with non-AI controls based on age, gender, provider, and indications (screening, surveillance, and diagnostic) in a (1:1) ratio.
Adenoma Detection Rate (ADR), Polyp Detection Rate (PDR), Polyps per Colonoscopy (PPC), and Adenoma Per Colonoscopy (APC) in AI cases and non-AI controls were then calculated and compared.
Results: The final analysis included 4028 patients (2014 cases, 2014 controls) with adequate bowelpreparation.
ADR was significantly higher in AI assisted group (38.6%) vs control (34.2%) (RR = 1.129, 99% CI, 1.013 to 1.257). PDR was also significantly higher in AI assisted group (67.2%) vs control (59.4%) (RR = 1.130, 99% CI, 1.062 to 1.202). Mean APC was significantly higher in AI group (0.406) vs control (0.359) (RR = 1.131, 95% CI, 1.046 to 1.223). PPC was also significantly higher in AI assisted group (5.276) vs control (4.452) (RR = 1.161, 99% CI, 1.115 to 1.208).
Discussion: Our study shows that AI-assisted colonoscopy is associated with an increased ADR, PDR, PPC, and APC ratios. The higher ADR translates to lower rates of interval colorectal cancer and improved patient outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kapil Nayar indicated no relevant financial relationships.
Abdelrahman Yakout indicated no relevant financial relationships.
Bakheet Nader indicated no relevant financial relationships.
Patrick Sanchez indicated no relevant financial relationships.
Yan Yan indicated no relevant financial relationships.
Yuting Huang indicated no relevant financial relationships.
Manar Al Jawish indicated no relevant financial relationships.
Michael Wallace: Fujifilm Medtronic Endostart Endiatix – Consultant.
Vivek Kumbhari: Fujifilm – Consultant. medtronic – Consultant. microtech – Consultant.
Kapil D. Nayar, MD1, Abdelrahman Yakout, MD2, Bakheet Nader, MBBCh, PhD2, Patrick S. Sanchez, 2, Yan Yan, MBBS, PhD2, Yuting Huang, MBBS, PhD2, Manar Al Jawish, MD2, Michael B. Wallace, MD, MPH2, Vivek Kumbhari, MBChB, PhD2. P0429 - The Impact of Real Time Artificial Intelligence Enhanced Colonoscopy: A One Year Performance Review, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
