Sunday Poster Session
Category: Colorectal Cancer Prevention
P0431 - Lost in Translation: Deciphering the Barriers to Colorectal Cancer Screening Among Spanish Speaking Patients
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Brian R. Hughes, MD
University of Colorado Anschutz Medical Campus
Aurora, CO
Presenting Author(s)
Hannah Carr, MD1, Nicole Reub, MD2, Brian R. Hughes, MD1, Elena Lebduska, MD1, Laura Macke, MD1, Prashanth Francis, MD, PhD2
1University of Colorado Anschutz Medical Campus, Aurora, CO; 2University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: Colorectal cancer (CRC) screening disparities are pervasive in the US, particularly in minority populations. Nationally, Hispanic adults are less likely to receive adequate CRC screening than non-Hispanic adults. Limited English proficiency (LEP) and associated systemic barriers have been proposed as potential contributors to lower screening rates in this population. The aim of this study is to examine CRC screening disparities and identify potential barriers to screening.
Methods: We used electronic medical record (EMR) reporting to identify all patients aged 45-75 at four internal medicine clinics within a single academic health system, specifically identifying cohorts with primary language listed as English or Spanish. We then conducted manual chart review of the Spanish speaking cohort, examining the type of CRC screening offered and scheduling information.
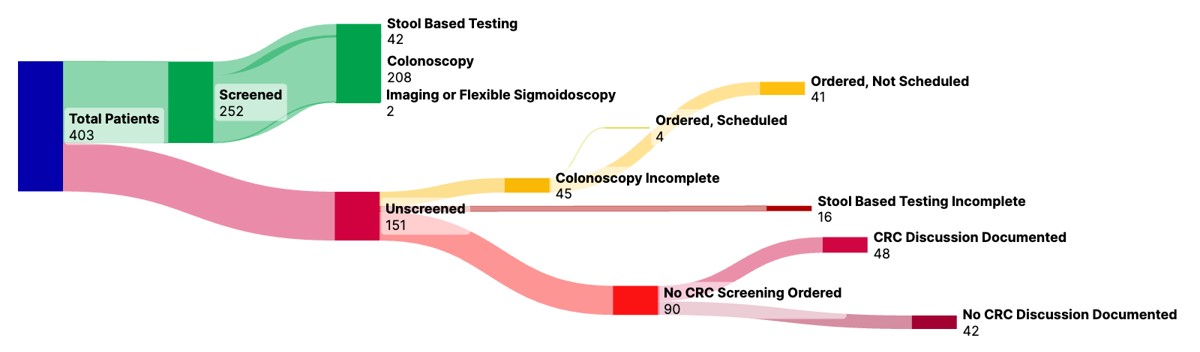
Results: 21,033 English speaking patients and 403 Spanish speaking patients with LEP were identified, 98.0% (395/403) of the latter identified as Hispanic or Latino/a. According to Epic reporting, 74.0% of English-speaking patients were screened for CRC compared to 62.1% of Spanish speaking patients. According to chart review, of the 252 Spanish-speaking patients who were screened, 83.3% (210/252) had a colonoscopy and 16.7% (42/252) had stool-based testing. Of unscreened patients, 27.8% (42/151) did not have a documented screening discussion or active order and 31.7% (48/151) had a discussion but no active order. Of unscreened patients, 27.1% (45/151) had an active colonoscopy order without appointment scheduled and 11.9% (18/151) had an active stool-based test order.
Discussion: Our data reflects nationwide trends in CRC screening disparities amongst Hispanic patients with LEP and are similarly driven by multi-factorial etiologies. Unlike previously published reports, our cohort had a uniquely high proportion of patients with incomplete CRC screening despite having active testing orders. We discovered that Spanish language instructions for stool-based testing were not available and language translation services were not provided when calling to schedule colonoscopy. These barriers are unique to patients with LEP and have spurred initiatives to improve interpreter services and the creation of Spanish language informational handouts. While this phase of our study shares the same limitations of prior retrospective chart reviews, it has informed changes already implemented and a forthcoming interview-based, qualitative analysis.
Disclosures:
Hannah Carr, MD1, Nicole Reub, MD2, Brian R. Hughes, MD1, Elena Lebduska, MD1, Laura Macke, MD1, Prashanth Francis, MD, PhD2. P0431 - Lost in Translation: Deciphering the Barriers to Colorectal Cancer Screening Among Spanish Speaking Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Colorado Anschutz Medical Campus, Aurora, CO; 2University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: Colorectal cancer (CRC) screening disparities are pervasive in the US, particularly in minority populations. Nationally, Hispanic adults are less likely to receive adequate CRC screening than non-Hispanic adults. Limited English proficiency (LEP) and associated systemic barriers have been proposed as potential contributors to lower screening rates in this population. The aim of this study is to examine CRC screening disparities and identify potential barriers to screening.
Methods: We used electronic medical record (EMR) reporting to identify all patients aged 45-75 at four internal medicine clinics within a single academic health system, specifically identifying cohorts with primary language listed as English or Spanish. We then conducted manual chart review of the Spanish speaking cohort, examining the type of CRC screening offered and scheduling information.
Results: 21,033 English speaking patients and 403 Spanish speaking patients with LEP were identified, 98.0% (395/403) of the latter identified as Hispanic or Latino/a. According to Epic reporting, 74.0% of English-speaking patients were screened for CRC compared to 62.1% of Spanish speaking patients. According to chart review, of the 252 Spanish-speaking patients who were screened, 83.3% (210/252) had a colonoscopy and 16.7% (42/252) had stool-based testing. Of unscreened patients, 27.8% (42/151) did not have a documented screening discussion or active order and 31.7% (48/151) had a discussion but no active order. Of unscreened patients, 27.1% (45/151) had an active colonoscopy order without appointment scheduled and 11.9% (18/151) had an active stool-based test order.
Discussion: Our data reflects nationwide trends in CRC screening disparities amongst Hispanic patients with LEP and are similarly driven by multi-factorial etiologies. Unlike previously published reports, our cohort had a uniquely high proportion of patients with incomplete CRC screening despite having active testing orders. We discovered that Spanish language instructions for stool-based testing were not available and language translation services were not provided when calling to schedule colonoscopy. These barriers are unique to patients with LEP and have spurred initiatives to improve interpreter services and the creation of Spanish language informational handouts. While this phase of our study shares the same limitations of prior retrospective chart reviews, it has informed changes already implemented and a forthcoming interview-based, qualitative analysis.
Figure: Methods of and Barriers to Colorectal Cancer Screening in Spanish-Speaking Patients at University of Colorado Internal Medicine Primary Care Clinics.
Disclosures:
Hannah Carr indicated no relevant financial relationships.
Nicole Reub indicated no relevant financial relationships.
Brian Hughes indicated no relevant financial relationships.
Elena Lebduska indicated no relevant financial relationships.
Laura Macke indicated no relevant financial relationships.
Prashanth Francis indicated no relevant financial relationships.
Hannah Carr, MD1, Nicole Reub, MD2, Brian R. Hughes, MD1, Elena Lebduska, MD1, Laura Macke, MD1, Prashanth Francis, MD, PhD2. P0431 - Lost in Translation: Deciphering the Barriers to Colorectal Cancer Screening Among Spanish Speaking Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
